口腔颌面颈部Castleman病:6例临床病例报告和文献复习
2020-03-18 何小桐 王琼 吴亚平 口腔医学
Castleman病(Castleman's Disease,CD)又称血管滤泡性淋巴组织增生或巨大淋巴结增生症,是一种罕见的、病因尚未明确的疾病,主要表现为慢性非特异性淋巴组织增生。临床上根据发病部
Castleman病(Castleman's Disease,CD)又称血管滤泡性淋巴组织增生或巨大淋巴结增生症,是一种罕见的、病因尚未明确的疾病,主要表现为慢性非特异性淋巴组织增生。临床上根据发病部位分为单中心型(unicentric CD,UCD)、多中心型(multicentric CD,MCD)和HHV-8+型。组织病理学上可分为透明血管型(hyaline-vascular CD,HVCD)、浆细胞型(plasma cell CD,PCD)以及混合型。该疾病多发生于纵隔、腹膜后,而较少发生于口腔颌面颈部,其临床诊断较为困难。本文收集了本院2007年至2017年收治并经病理明确诊断为口腔颌面颈部CD的6个病例,并结合文献分析口腔颌面颈部CD患者的发病特点、临床病理特征及治疗预后。
1.临床资料
1.1一般资料
患者资料如表1所示。本组病例中女4例,男2例。年龄10~49岁,平均年龄31.8岁。均因偶然发现无痛性包块入院。入院后系统检查无异常。查体均示腮腺或颈部无痛性包块,大小1 cm×2 cm至3 cm×5 cm不等,境界均清晰,质地软至中等偏硬,其余未见异常。
表1 本院6例颈部CD患者的临床资料
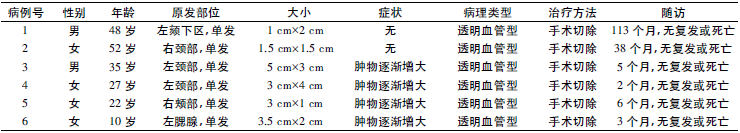
1.2辅助检查
患者均行血常规、尿常规、生化及X线胸片检查未见异常。CT检查均提示相应部位淋巴结肿大,质均匀,界清晰,考虑良性占位(图1)。
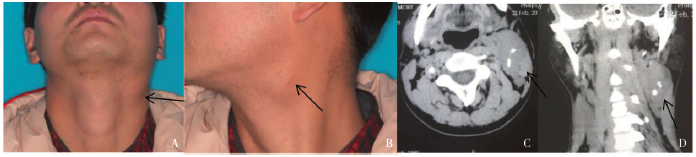
图1 典型颈部CD患者的临床照片及CT影像资料(男,35岁)。A、B:左颈部肿物的前面观(A)及侧面观(B);C、D:CT检查:水平位及冠状位CT提示颈部肿物占位病变,信号均匀,境界清晰
1.3治疗方法
排除全麻手术禁忌后,所有患者均于全麻下行“肿物切除术”。术后未予其他治疗,定期随访。
1.4病理及免疫组化结果
肉眼观察可见肿物包膜完整,切面实性、均质,剖面可呈灰白、暗红色、黄色。镜下可见淋巴组织及血管增生,呈淋巴滤泡样结构,小淋巴滤泡围绕滤泡中心呈“同心圆”或“洋葱皮样”结构,生发中心大部分消失,滤泡间毛细血管增生。免疫组化:CD3(+),CD20(+),CD34(+)。本组6例患者术后常规病理诊断均为HVCD(图2)。

图2 HVCD组织病理图。A:病理组织细胞学切片显示淋巴滤泡生发中心,周围淋巴细胞呈同心圆排列,内可见血管玻璃样变性;B、C、D:免疫组化显示CD3(B),CD20(C),CD34(D)滤泡间阳性表达
1.5随访结果
6例患者随访2个月至9年不等,均未出现肿物复发。
2.讨论
2.1CD流行病学特点
1956年Castleman首次回顾总结了11例发生于纵隔部的慢性淋巴结增生疾病,并命名为Castleman病。CD可发生于任何年龄,该疾病好发部位依次为胸部、颈部、腹盆部、腹膜后及腋窝、腹股沟等淋巴组织聚集区。CD在任何年龄均可发病,平均发病年龄在34岁左右,以10~45岁常见,其中MCD发病年龄较UCD晚,发病年龄多集中在50岁以上,男女间发病率无明显差异。
在临床上,口腔颌面颈部CD患者多发于颈部,表现为局域性单个或多个淋巴结增生,病理表型多为HVCD。与以往文献报道结果相似,这6例患者均为UCD,平均年龄31.8岁,年龄分布在10~52岁之间,男女比例为1∶2。其中3例发生于颈部,另外3例分别发生于颊部、腮腺及颏下。
2.2CD发病机制
该疾病发生原因及病因机制尚未明确,可能与HHV-8病毒感染、白细胞介素(IL-6)升高、血管内皮生长因子(VEGF)有关。现认为:HHV-8病毒诱导IL-6类似物VEGF表达,从而促进B细胞增殖、新生血管形成,而B细胞又会进一步增加IL-6表达,从而促进疾病发展。此外,IL-6细胞因子已成为CD公认的致病因子之一。研究指出在伴全身症状的UCD患者淋巴结中,能检测出IL-6表达水平异常增高,而手术切除术后,UCD患者的血清IL-6水平逐步降低。降低MCD患者IL-6水平后CD症状可以得到显著缓解。
2.3CD病理特征
根据病理学特征CD可分为透明血管型(HVCD)、浆细胞型(PCD)和混合型。①HVCD:镜下表现为淋巴滤泡增生,生发中心变小或消失,滤泡间可见增生毛细血管,管壁玻璃样变,以及树突状细胞和嗜酸性粒细胞浸润,周围小淋巴细胞增生,围绕生发中心呈同心圆排列,表现为特征性“洋葱皮”样结构。②PCD:PCD与HVCD病理学特征相似,但PCD组织学特点表现为滤泡间大量成熟的浆细胞,小血管成分较HVCD少且玻璃样变不明显。③混合型:组织学上同时具备HVCD及PCD的特征。除此之外,HHV-8+型PCD具有独特的病理组织学特点,表现为生发中心边界不清,毛细血管大量增生,滤泡间散在分布大量浆母细胞,因此又称浆母细胞型。此型PCD在一定程度上与弥漫性大B淋巴瘤的发生及发展有关。本文中6例患者术后病理学观察符合典型HVCD组织病理学特点。
2.4CD临床表现
根据CD临床表现特征可分为UCD和MCD。在临床上,MCD患者若合并HIV感染,通常HHV-8也表现为阳性,同时,少部分HIV-患者也能检测出HHV-8+。有研究者提出,MCD患者若检测出HIV及HHV-8均阴性且无法明确病因,统一归类为特发性MCD(idiopathic multicentric castleman disease,iMCD)。90%的UCD患者病理表现为HVCD,此类患者一般不伴有全身症状,仅表现为局部无痛性淋巴组织增生或肿物压迫症状。但另有大约10%的UCD患者,病理诊断为PCD,此类患者通常伴有明显系统性全身症状,如高热、体重减轻,脾肿大等,实验室检查可表现为贫血、高蛋白血症等。
本文收集的6例口腔颌面颈部UCD的患者,病理诊断均为HVCD,临床表现为渐大无痛肿物,实验室检查结果均未见明显异常。绝大部分MCD患者常伴有明显系统全身症状,包括高热、夜间盗汗、体重降低及乏力疲劳等。除了头颈部之外,全身其他淋巴组织集中区,如腹股沟、腋窝、腹部等均可能出现淋巴增生,同时伴随肝脾肿大、下肢水肿等。此外,HIV相关型MCD通常伴随其他恶性肿瘤,如卡波西肉瘤、原发性渗出性淋巴瘤,而这些伴随疾病的致病机制与HHV-8+有关。
2.5CD的诊断及鉴别诊断
CD明确诊断主要依靠病理检查。通常T淋巴细胞标记物CD3、CD43和CD45表现为滤泡间弥漫阳性或多数细胞阳性,B淋巴细胞标记物CD20、CD45和CD79a表现为滤泡间阳性。HVCD与PCD的区别在于:HVCD中血管内皮细胞标记物CD34、CD31弥漫阳性,说明血管明显增生,而PCD中滤泡内血管增生不明显,大量CD138阳性标记的浆细胞呈“铺单样排列”。此外,若出现滤泡内CD21、CD68弥漫阳性,呈现滤泡树突状细胞(FDC)大量异常增生,则病变可能进一步发展至FDC肉瘤。
常规影像学检查表现为类圆形软组织密度肿块,局部可发生钙化。本组病例中所有患者均行CBCT检查,表现为均匀或不均匀团块,未见钙化,缺乏特异性,难以明确诊断。免疫组化结果示CD3(+)、CD20(+)及CD34(+),表明T淋巴细胞、B淋巴细胞及血管大量增生,结合病理最终明确诊断为HVCD。Castleman病在临床表现缺乏特异性,与之相鉴别的疾病众多,其中良性肿瘤包括:多形性腺瘤、颈动脉体瘤、Warthin瘤、神经鞘瘤、炎性淋巴增生等,相关影像学检查可辅助鉴别诊断。
一般来说,CT或MRA可提示颈动脉体瘤多位于颈内外动脉分叉处,并将血管向周围推挤,而CD肿物往往位于淋巴结链上,且血供来源丰富,往往可与大部分良性肿瘤相鉴别;超声多用于鉴别CD和腮腺区良性肿瘤,多形性腺瘤往往呈现多边形、界清、无囊样的结构,Warthin瘤表现为囊性无回声区,而CD一般表现为一致的低回声区,并具有良好的穿透性。
CD与恶性肿瘤的鉴别诊断包括霍奇金淋巴瘤、滤泡型淋巴瘤、腺样囊性癌、转移淋巴结等。恶性肿瘤患者在临床上常伴有疼痛、局部感觉异常、神经麻痹及有短期内肿物迅速增大史,而转移淋巴结的患者通常可以发现原发肿瘤。除了临床鉴别诊断,还可考虑利用冷冻切片及细胞学鉴别诊断,霍奇金淋巴瘤及滤泡型淋巴瘤通常无毛细血管增生及透明变性滤泡的形成,细胞学上常表现出异型性,而CD恰与其相反,表现为血管大量增生和较小可能的细胞异型性。
2.6CD治疗及预后
在治疗及预后上UCD与MCD有明显差异。对于UCD来说,治疗多以手术切除为主,预后较好。本文报道的6例口腔颌面颈部UCD患者,在经过手术完整切除后,随访2个月至9年不等,均无复发。亦有学者提出利用放疗来治疗UCD患者,针对CD的放疗方法分为根治性放疗及术前辅助性放疗,根治性放射疗法适用于无法耐受手术、拒绝手术治疗的患者;而术前辅助性放疗适用于肿瘤过大、经过放疗后肿瘤明显缩小的患者,从而利于手术完全切除肿物。
MCD治疗方法有很多,目前尚无标准治疗方案,一般以化疗为主,常选择CHOP方案,也有利用免疫调剂(干扰素)、IL-6抗体及CD20单克隆抗体治疗者。针对HIV+的患者,由于存在免疫抑制大剂量化疗的风险较大,可考虑利用siltuximab(IL-6抗体)及tocilizumab(IL-6受体抗体)治疗。由于MCD患者常伴发全身症状,疗效和预后有较大差异,通常伴有AIDS、POEMS综合征者或因年龄过大无法耐受化疗者预后较差。
综上所述:口腔颌面颈部CD较为罕见,确诊依赖病理,临床上以UCD为主,治疗主要是手术切除,预后良好,而MCD常伴全身症状,预后不佳,需长期随访。
原始出处:
何小桐,王琼,吴亚平,王东苗,王琰玲,程杰.口腔颌面颈部Castleman 病: 6 例临床病例报告和文献复习[J].口腔医学,2019(03):246-250.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
103
#AST#
49
#EMA#
54
#Castleman病#
72
#病例报告#
109
#颈部#
74
#Cas#
58