JAHA:高血压患者左室扭转与主动脉硬化的关系!
2018-03-01 xing.T MedSci原创
由此可见,高血压患者左室基底部扭转与主动脉硬化增加及舒张功能改善有关。这些变化可能弥补主动脉硬化对左室舒张的有害影响。
左心室扭转在心脏效率中起关键作用。在高血压患者中,主动脉硬化增加心脏后负荷。然而,关于左室区域性收缩与主动脉硬化之间的联系却知之甚少。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估这些关系及其对左室舒张功能的贡献。
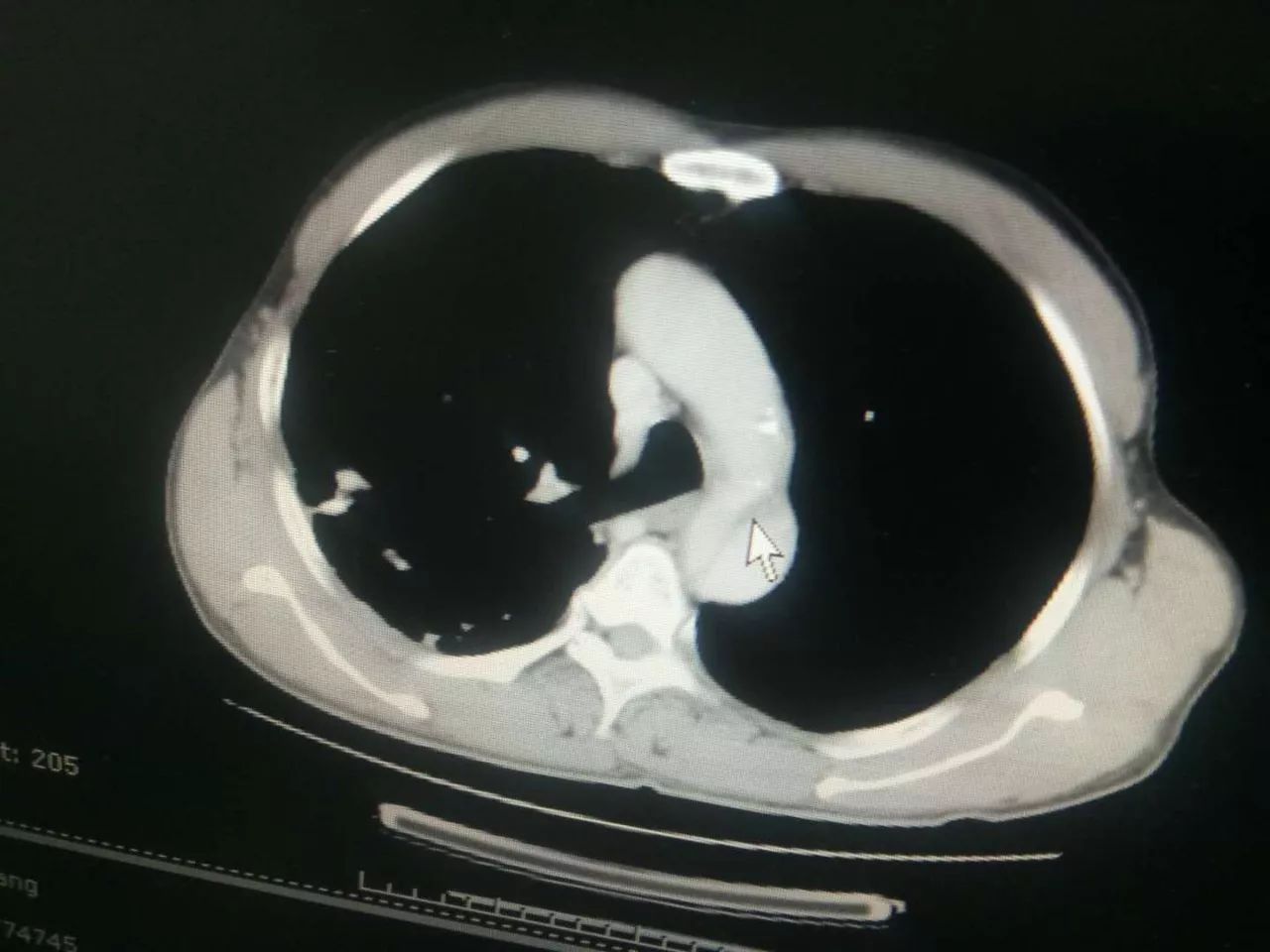
该研究纳入了血压正常个体和高血压患者,他们左室射血功能正常。研究人员测量了受试者心尖、基底部和整体左室旋转速度和左心室整体纵向应变(2维斑点追踪超声心动图)。通过颈动脉脉搏波速度计算主动脉硬化程度,并从舒张早期二尖瓣环运动计算左室舒张功能。通过计算基底部或心尖未扭转/扭转率比值来评估主动脉硬化与左室扭转参数之间的关系。
高血压患者左室扭转和未扭转率均大于血压正常的个体,因为增加的基底部扭转率(P<0.001)和未扭转率(P<0.001)。左室舒张功能下降(舒张早期二尖瓣环运动=7.4±1.9 vs. 10.4±2.3 cm/s,P<0.001)。在整个人群中,基底部未扭转率随主动脉硬化(R=0.43;P<0.001)和左室舒张(R=0.41;P=0.001)而增加。基底部未扭转/扭转率的比值与颈‐股脉搏波速度呈正相关,而且在高血压组明显高于对照组,并与颈动脉‐股脉搏波速度呈正相关(P<0.001)。这些结果与年龄、治疗、平均血压和左室质量无关。
由此可见,高血压患者左室基底部扭转与主动脉硬化增加及舒张功能改善有关。这些变化可能弥补主动脉硬化对左室舒张的有害影响。
原始出处:
Jean‐Barthelemy Gnakamene,et al. Left Ventricular Torsion Associated With Aortic Stiffness in Hypertension.JAHA.2018. https://doi.org/10.1161/JAHA.117.007427
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#左室扭转#
51
#主动脉硬化#
60
#AHA#
53
#主动脉#
59
#高血压患者#
75
学习知识了.很有帮助
87
VB哈哈哈还好还好哈
103