PLoS One: 卒中后睡眠呼吸障碍与卒中部位无关?
2017-04-22 phylis MedSci原创
缺血性脑卒中患者睡眠呼吸障碍(SRBD)很常见,且与不良预后相关。卒中后SRBD可能是中枢神经系统具体结构损伤的一个直接后果。然而,是否缺血性卒中的具体位置引起SRBD是尚不清楚。因此研究者研究了SRBD与缺血性病变部位的关系。方法:卒中单元治疗的急性缺血性卒中患者纳入前瞻性观察研究。所有患者在卒中急性期均行磁共振成像(MRI)和多导图睡眠监测。SRBD是指睡眠呼吸暂停低通气指数(AHI)≥10。
缺血性脑卒中患者睡眠呼吸障碍(SRBD)很常见,且与不良预后相关。卒中后SRBD可能是中枢神经系统具体结构损伤的一个直接后果。然而,是否缺血性卒中的具体位置引起SRBD是尚不清楚。因此研究者研究了SRBD与缺血性病变部位的关系。
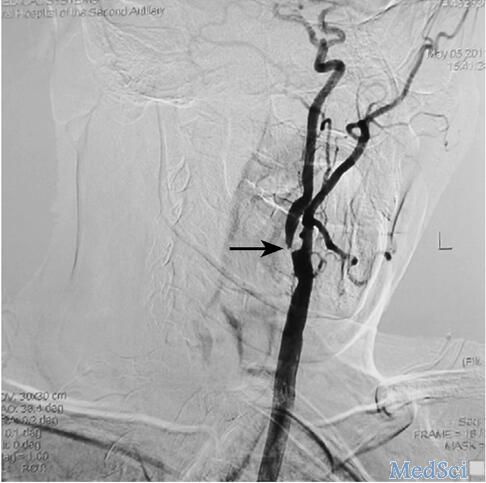
方法:卒中单元治疗的急性缺血性卒中患者纳入前瞻性观察研究。所有患者在卒中急性期均行磁共振成像(MRI)和多导图睡眠监测。SRBD是指睡眠呼吸暂停低通气指数(AHI)≥10。应用MRI标准影像图确定,存在或不存在SRBD的卒中患者梗死部位的可能分布情况。采用Logistic回归分析进行组间比较。
结果:共纳入142名患者,86(59%)例患者存在SRBD。SRBD组患者年龄、体重指数和高血压高于非SRBD组。梗死部位与SRBD之间无统计学意义。
结论:研究显示脑卒中患者脑卒中部位与SRBD无相关性,而SRBD的风险因素与SRBD显著相关。鉴于脑卒中患者SRBD的高患病率,这些研究结果表明,SRBD的发生不是由中枢神经系统结构的损伤引起,可能是卒中患者存在SRBD的危险因素。研究结果可以用来确定从多导图睡眠监测中获益的卒中患者。
原文出处:
Fisse AL, Kemmling A,et al. The Association of Lesion Location and Sleep Related Breathing Disorder in Patients with Acute Ischemic Stroke. PLoS One. 2017 Jan 30
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#卒中后#
75
#Plos one#
82
#呼吸障碍#
82
#睡眠呼吸#
80
学习了,谢谢分享
113
#睡眠呼吸障碍#
100