Diabetologia:糖尿病妊娠是子代心脏功能障碍的新危险因素
2021-11-20 从医路漫漫 MedSci原创
有人认为,宫内环境对后代健康的影响可能受到出生后环境因素的调节,如生长和营养。
有几项研究调查了母亲高血糖对后代健康的影响。有人认为,宫内环境对后代健康的影响可能受到出生后环境因素的调节,如生长和营养。关于妊娠期间糖尿病影响的数据大多集中在后代的代谢状态,如肥胖和糖尿病,而关于其对心脏功能影响的研究较少。胎儿期的不良影响可能会增加以后心血管结局风险,但潜在的机制仍不充分了解,尽管有关BP影响的证据正在慢慢出现。
丹麦最近的一项队列研究表明,如果母亲在怀孕前或怀孕期间有糖尿病,40岁以下的儿童和成年人患早期心血管疾病的风险更高。母亲妊娠期间有糖尿病的患儿血压高于对照组患儿。有趣的是,在母亲有糖尿病的孕期,男性后代似乎更容易受到高血压的影响。报道了妊娠前高血糖大鼠胎儿的心功能障碍和基因表达改变。大鼠子宫高血糖灌注引起胎儿心脏间隔过度生长。本研究的目的是探讨糖尿病妊娠对成年雄性后代心脏健康的影响。
研究方法:
选定的转基因Tet29大鼠模型是在Sprague-Dawley背景下产生的,携带一种产生干扰胰岛素受体表达的shRNA的DNA结构。由此产生的胰岛素受体被多西环素(DOX)诱导下调,并产生高血糖和高胰岛素血症。这一机制受到严格的调控;当DOX治疗停止时,胰岛素受体的下降将会减弱。在平均室温22°C、湿度55±15%、光线黑暗、周期12/12h的标准条件下进行动物饲养。大鼠可以随意进食(NC:54%碳水化合物,36%蛋白质,10%脂肪,V1324-300,Ssniff Spezialdiäten,Soest,德国;HFD:35%碳水化合物,20%蛋白质,45%脂肪,D12451i,Research Diets,New Brunswick,美国)。
实验结束后,在1.5%异氟醚麻醉下断头处死大鼠。为了在妊娠期诱导糖尿病环境,转基因Tet29母鼠(n=14)按体重1.5 mg/kg口服多柔比星(DOX)。与野生型(WT)雄性交配开始时,Tet29雌性的高血糖水平达到约16.65 mmol/l。为了防止胚胎毒性/胎儿毒性,当雌性出现阴道堵塞(定义为怀孕第1天)时,停止服用DOX。平均到受孕前服用DOX 9.8天,但DOX对血糖水平的影响在整个妊娠期间持续存在(图1b)。将12只WT母鼠与Tet29转基因雄鼠交配,同时给予1.5 mg/kg体重的DOX处理。在这里,受孕前服用DOX的平均时间为9.3天。妊娠结束时,采集血液样本进行进一步分析。同时培育WT哺乳,以进行不含DOX的母乳喂养。分娩的后代在妊娠第22天需要剖腹产,幼崽由WT哺乳饲养,以避免被高血糖乳汁哺乳引起偏倚。幼崽跟踪到成年,最后接受HFD饮食。为此,我们以随机方式对每组进行了分配。因此,将正常或高血糖孕妇分为正常妊娠组(n=8,8)和高血糖妊娠组(n=15,10),分别饲喂NC(n=8,8)和HFD(n=15,10)。在36周龄时,处死后代,称重,采血,取出器官,称重并冷冻保存。这项研究中动物的代谢特征,包括GTT、ITT和远程连续血糖测量已有报道。在这里,我们将重点放在对动物的心脏分析上。通过超声心动图、循环因子、免疫组织化学和心脏基因表达来评估心脏表型。
研究结果:
正常饲喂食物时,成年糖尿病和正常血糖大鼠的子代在心功能、基因表达和血浆脑钠肽水平上无明显差异。有趣的是,在高脂饮食条件下,糖尿病妊娠成年子代整体心脏纵向改变(−14.82±0.59vs−16.60±0.48%)和周向应变(−23.40±0.57vs−26.74±0.34%)降低,相对壁厚(0.53±0.06vs 0.37±0.02)增加,心肌基因表达改变,心肌细胞增大(106.60±4.14vs 87.94±1.67μm)。心脏免疫细胞积聚(10.27±0.30vs6.48±0.48个/fov),在高脂饮食的条件下,血浆脑钠肽水平(0.50±0.12vs0.12±0.03 ng/ml)高于正常血糖的子代(0.50±0.12vs0.12±0.03 ng/ml)。高脂肪饮食组的血压、尿白蛋白、血糖和体重没有变化。
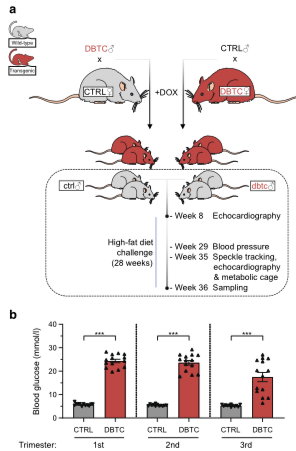
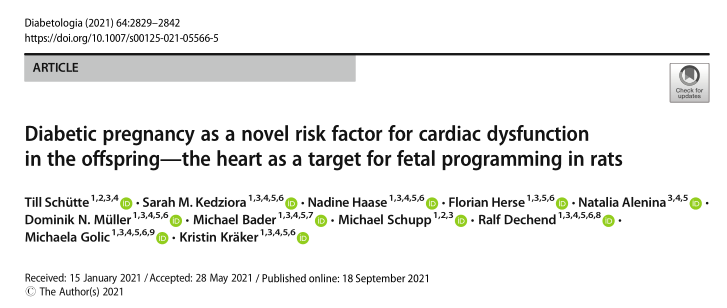
图1 转基因大鼠模型与母体妊娠期血糖的实验交配方案及随访。双亲WT雌鼠(CTRL)和转基因Tet29(TG)雌鼠(DBTC)经饮水预先给予1.5 mg/kg DOX。WT雌性与TG雄性交配(DBTC),TG雌性与WT雄性交配(CTRL)。一旦登记有阴道塞子,就停止DOX治疗。对正常血糖(Ctrl)和糖尿病(DBTC)大鼠的雄性WT后代进行随访(虚线框)。在饮食挑战前8周进行超声心动图检查,持续28周。血压测量是在29周龄时进行的。在35周龄时进行超声心动图、深度斑点追踪分析和代谢笼检查。在挑战结束时(36周龄)提取样本(A)。TG雌性在怀孕的每个三个月期间累积的平均血糖水平显著较高(B)。正常血糖组(n=12)和糖尿病组(n=14),均值±SEM,非配对t检验(B),*p≤0.001。

图2 饮食调整后STE对子代的深入分析。左心室的组织动力学测量是在多个单点绘制的心内膜图上进行的。节段值总结为六个定义区域(绿色:后基部,白色:后中部(部分被黑线遮挡),青色:后尖部,蓝色:前基部,黄色:前中部,粉红色:前尖部,黑色:平均值),全局值按三个心动周期的平均值计算(VevoSTrain软件,版本2.2.0)(A)。与对照组相比,饲喂NC的DBTC子代GLS、GCS和GRS(b-d)及其比率(GLSR、GCSR、GRSR)(e-g)没有改变。与对照组相比,饲喂HFD后,DBTC子代GLS和GCS(b,c)显著降低,而GRS(D)无明显变化。HFD(E)后GLSR降低。HFD后残余周向应变率和径向应变率(f,g)没有降低。正常血糖(ctrl,NC;b,en=7;c,d,f,gn=5;HFD;b,en=7;c,n=5;d,f,gn=6)和糖尿病大鼠(DBTC,NC;b,en=8;c,n=6;d,f,gn=7;HFD;B-f,n=5),长轴测量GLS/R,短轴测量GRS/R,35周龄超声心动图,非配对t检验(b,c,d,e,g)和Mann-WhitneyUtest(F),均值±SEM,*p≤0.05,*p≤0.001
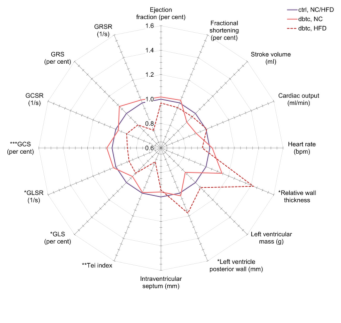
图3 饮食障碍后代的聚合基础超声心动图和深入分析。正常血糖母鼠雄性WT子代数据归一化为1(紫线,NC/HFD,n=7/7),然后合并。糖尿病妊娠的雄性WT后代与对照妊娠的雄性WT后代进行比较,不受食物(NC或HFD)的影响。雄性WT糖尿病子代饲喂NC(实线,n=8)或HFD(虚线,n=5)的相对改变。超声心动图在35周龄时进行评估。相对平均值,非配对t检验和Mann-Whitney U检验,*p≤0.05,**p≤0.01,*p≤0.001

示HFD致病后代心脏基因表达谱。通过qPCR获得HFD挑战后心尖的基因表达谱,并以热图(用色标显示的表达)显示绝对值(A)和选定的基因(b-j),参照36B4管家基因表达。与对照组相比,DBTC后代表现出明显不同的基因表达谱。正常血糖(Ctrl,n=11)和糖尿病大鼠(DBTC,n=8)的后代,36周龄时进行qPCR,非配对t检验(b,c,e,f,g,h,i,j)和Mann-WhitneyU检验(D),单值(A),用X(A)标记的异常值,均数±SEM(b-j),*p≤0.0 5,**p≤0.0 1,*p≤0.001
子代心脏组织的免疫组织化学研究。心脏横切面用WGA染色测量心肌细胞周长,与ctrl(A)相比,高脂饲料喂养的DBTC子代心肌细胞周长显著增加。测量COL1以比较血管周围纤维化面积与血管壁面积的关系。与对照组(B)相比,DBTC子代没有改变。与ctrl(C)相比,DBTC子代检测到的CD68阳性细胞数ED1显著增加。正常血糖(Ctrl,NC/Hfd,n=6)和糖尿病大鼠(DBTC,NC/Hfd,n=6/6)的雄性WT后代,标尺WGA/COL1/ED1 10/100/20μm,非配对t检验,均值±SEM,**p≤0.01,*p≤0.001
结论:糖尿病妊娠大鼠只有在高脂饮食后才会导致成年大鼠子代的心功能障碍、左心室肥厚和促炎状态改变。糖尿病妊娠本身并不足以损害成年雄性后代的心肌功能和基因表达。这表明高脂饮食对糖尿病妊娠后大鼠子代心脏功能障碍的发生具有重要意义。糖尿病妊娠是一种新的心脏危险因素,当存在其他危险因素时,如高脂饮食,这种因素与心脏改变更相关。
原文出处:
Schütte T, Kedziora SM, Haase N,et al.Diabetic pregnancy as a novel risk factor for cardiac dysfunction in the offspring-the heart as a target for fetal programming in rats.Diabetologia 2021 Sep 18
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#子代#
106
#BET#
107
#DIA#
86
#心脏功能障碍#
86
学习了
89
学习了~
105
学习了!
135
#心脏功能#
104
#功能障碍#
76
大影响人们的生活质量。大多数LSS患者表
163