Lancet:非低风险乳腺导管原位癌的放疗剂量和分割方案
2022-08-09 MedSci原创 MedSci原创
对于切除后的非低危乳腺导管原位癌患者,全乳放疗后对肿瘤床进行强化放疗可减少局部复发率
导管原位癌 (DCIS) 保守手术后全乳照射 (WBI) 可使局部复发率减半,因此,术后放射治疗是 DCIS 患者保乳治疗不可或缺的一部分。有研究发现,WBI 后强化肿瘤床治疗可显著降低大部分侵袭性乳腺癌患者的局部复发率,但尚无随机试验证实。
该研究调查了 WBI 后强化肿瘤床放疗是否可以改善非低风险 DCIS 患者的预后,并评估了非低风险 DCIS 患者的放疗剂量分割敏感性。
这是一项在多个国家开展的国际性、随机、非盲的3期临床试验,招募了年满18岁的单侧的组织学明确诊断的接受保乳手术治疗的非低风险 DCIS 女性患者,随机(1:1:1:1)分成四组:无肿瘤床强化 vs 常规 WBI 后强化 vs 大分割 WBI 后强化,或随机(1:1)分至无强化 vs 每次常规 WBI 后强化 vs 每次大分割 WBI 后强化。常规 WBI 总剂量是 50Gy,分成25次,大分割 WBI总剂量是42.5Gy,分成16次。强化剂量是16Gy,分成8次。主要终点是局部复发的时间。
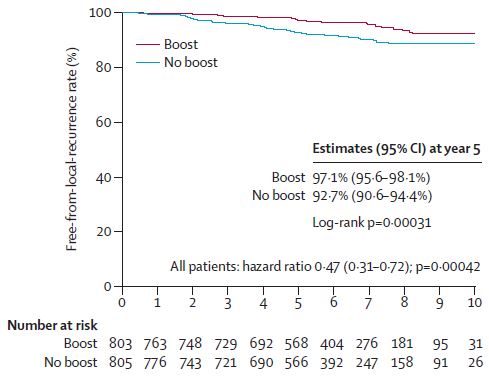
有无强化放疗患者的无局部复发生存率
2007年6月25日-2014年6月30日,共1608位患者被随机分至无强化组(805位)或强化组(803位)。831位患者进行了常规 WBI,777位患者进行了大分割 WBI。中位随访了6.6年。无强化组和强化组的5年无局部复发生存率分别是92.7%和97.1%(HR 0.47,p<0.001)。强化组有更高的≥2级的乳腺疼痛(10% vs 14%)和硬结率(6% vs 14%,p<0.001)。
综上,对于切除后的非低危乳腺导管原位癌患者,全乳放疗后对肿瘤床进行强化放疗可减少局部复发率,但同时会增加 2 级及以上毒性的发生率。该研究是首个证实这类患者术后WBI后强化放疗可改善局部控制情况的随机试验。
原始出处:
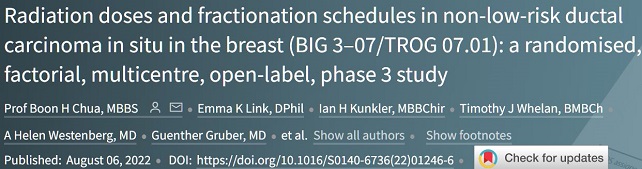
Boon H Chua, et al. Radiation doses and fractionation schedules in non-low-risk ductal carcinoma in situ in the breast (BIG 3–07/TROG 07.01): a randomised, factorial, multicentre, open-label, phase 3 study. Lancet. August 06, 2022. https://doi.org/10.1016/S0140-6736(22)01246-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
132
#原位癌#
76
#乳腺导管原位癌#
80
lancet上果然牛,感谢梅斯更新及时
79