盘点:7月NEJM病例汇总
2017-08-03 MedSci MedSci原创
7月刚刚过去,NEJM又收录了一些罕见的病例报告,这里梅斯小编汇总了一下,与大家一起分享。【1】海绵状血管畸形患者为一位59岁的男性,因渐进性头痛恶化一年而到门诊就诊。神经系统检查正常;皮肤检查发现多个角化丘疹和结节性皮肤病变。共振成像发现大脑中发现许多病变符合海绵状血管畸形的表现,病变累及大脑半球、小脑、脑干(如图A所示T2加权、快速场回波图像,以图B血氧水平依赖的图像;P代表后部)。海绵状
7月刚刚过去,NEJM又收录了一些罕见的病例报告,这里梅斯小编汇总了一下,与大家一起分享。
患者为一位59岁的男性,因渐进性头痛恶化一年而到门诊就诊。神经系统检查正常;皮肤检查发现多个角化丘疹和结节性皮肤病变。
共振成像发现大脑中发现许多病变符合海绵状血管畸形的表现,病变累及大脑半球、小脑、脑干(如图A所示T2加权、快速场回波图像,以图B血氧水平依赖的图像;P代表后部)。
海绵状畸形主要发生在大脑,但也可在皮肤、脊髓和视网膜中发现。一部分脑海绵状血管畸形患者是无症状的,而另一些则伴有神经症状,如癫痫发作、头痛,甚至出现致死性脑出血。脑海绵状血管畸形可能是散发性的或家族性的。患者母亲和外祖父有类似于该患者的皮肤病变,但没有进行脑部成像。
对该患者进行遗传分析显示,KRIT1基因突变(也叫CCM1)是与家族性海绵状血管畸形综合征诊断相一致。由于大量脑海绵状血管畸形存在,神经外科治疗并不是一种选择的治疗方案。
该患者仍有间歇性头痛,可通过β受体阻滞剂治疗部分缓解。但该患者也发生了轻度认知减退和记忆缺失。
【2】眼睑下垂
患者为一位27岁的女性,因眼睑下垂,并且在下午进一步恶化的病史而到三级医疗中心就诊。该患者报告没有其他神经症状,如复视、无力、肢体麻木、易疲劳、语音和吞咽障碍等。
该患者瞳孔双侧对称、圆的、对光分数和调节反射正常,左侧眼睑明显下垂(如图A所示),持续向上凝视眼睑下垂加重。右眼睑似乎不受影响;然而,手动提起左侧眼睑引起右侧上睑下垂。实验室检查显示乙酰胆碱受体抗体水平为4.56nmol/L(正常值<0.05nmol/L),这一发现与重症肌无力诊断一致。
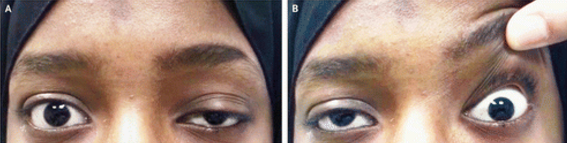
在眼睑的上睑提肌有大致相等的神经支配。在不对称性上睑下垂的情况下,增加运动冲动,以弥补下垂受影响更多的一侧,从而使两个眼睑相平,这就足以掩盖受影响较小的轻度下垂一侧眼睑。手动提起受影响的眼睑,需要保持眼睑抬高得到缓解,这些运动冲动减弱,从而揭示了对侧眼睑下垂的机制。
该患者患有重症肌无力,但这种现象可能发生在那些由于任何外部原因而导致眼睛不对称的上睑下垂的患者上。该患者服用吡啶斯的明和泼尼松治疗,使上睑下垂得到了迅速改善,并且在2年的随访中该患者一直保持良好。
【3】胆石症
患者男性,60岁,肝硬化与结肠癌史,因此接受了右半结肠切除术,因发烧而求治与急诊科。
患者无腹泻、呕吐或腹痛表现,体温为38.5°C,腹部没有压痛。
实验室研究显示,白细胞计数为12300每立方毫米,(正常范围3600-11000),总胆红素水平为2毫克每分升(34.2μ摩尔每升)(正常范围0.2-1.3毫克每分升[ 3.4-22.2μ摩尔每升]),患者由于肝病原因基线总胆红素水平为2毫克每分升。转氨酶和碱性磷酸酶水平,以及尿检结果均在正常范围内。入院时血培养大肠杆菌阳性。
计算机断层扫描以确定是否存在腹腔感染,结果并没有发现脓肿、腹水或结肠炎,但扫描结果显示多个小的、圆的钙化结石(图A和B)。
虽然并没有发现导致菌血症的原因,但是在患者体温正常后的第一个48小时内给予抗生素治疗。由于患者存在肝硬化因此行胆囊切除术风险较高而放弃实施。患者接受了一个疗程的抗生素治疗,并在出院后11个月的随访中无不良状况发生。目前的监测还没有发现结肠癌复发。
【4】韦尼克脑病
患者女性,28岁,妊娠11周时手术流产,2周后出现眩晕、意识混乱和跌倒。
患者怀孕期间并发持续性妊娠剧吐。体格检查显示,患者自发的兴奋性眼球震颤,凝视诱发眼震和步态共济失调。患者并没有眼肌麻痹。大脑磁共振成像显示,中脑导水管周围灰质(图A,箭头所示)和双侧丘脑(图B,箭头所示)出现T2高信号。
最终诊断为韦尼克脑病。韦尼克脑病的原因是由于妊娠剧吐导致的硫胺(维生素B1)缺乏症;当然也可在饮酒、减肥手术或营养不良的情况下发生。如果不经治疗,韦尼克脑病可导致昏迷或死亡。韦尼克脑病可存在眼球运动异常的表现,包括凝视诱发眼震,自发的兴奋性眼球震颤,以及水平或垂直性眼肌麻痹。静脉注射硫胺素速度过快,患者或可出现水平前庭眼反射障碍。
最终患者接受大剂量静脉注射硫胺素,减轻了眼球运动异常和共济失调。
【5】阻塞性支气管石
患者女性,68岁,因出现呼吸急促、喘息、干咳、发烧和发冷3天而就诊于急诊。
检查发现,患者正常呼吸时,血氧饱和度是96%。患者左下叶肺听诊出现爆裂声。胸部CT扫描显示,左下叶支气管出现阻塞性支气管石(图A箭头),周围出现毛玻璃样和斑片状实变(图B)。支气管镜检查发现,一个松散的支气管石阻塞在左下叶支气管近端(图C)。使用支气管镜轻轻取出支气管石,大小约为1*1.45厘米(图D)。

支气管石最常是由于支气管周围淋巴结钙化并迁移到支气管管腔形成。慢性肉芽肿性感染(如组织胞浆菌病或肺结核)后可引起淋巴结钙化。对患者的支气管肺泡灌洗液培养,显示结核分枝杆菌、细菌和真菌阴性。使用γ干扰素释放试验来检测患者既往结核杆菌暴露,结果显示阴性,血清学检测显示组织胞浆菌阴性。
患者最后接受抗生素治疗其阻塞性肺炎,经治疗其症状消失。
【6】HPV感染所致的严重跖疣
患者女性,25岁,曾接受原位心脏移植,因双脚出现广泛疣(图A)4年而就诊于一家整形外科诊所。

患者述其双脚疣状物是在心脏移植术后7年首次出现,导致严重的疼痛、肿胀和残疾。自接受心脏移植以来,患者一直接受霉酚酸酯和他克莫司进行免疫抑制治疗。患者曾接受外用水杨酸局部化学消融、局部氟尿嘧啶和二氧化碳激光治疗疣。
体格检查发现外生性疣状增生出现在双脚的足底表面的跖骨和足跟区域,同时伴有足部水肿。这些皮肤疣是由于患者感染了人乳头瘤病毒引起的。
患者接受了积极的减压治疗,然后外用西多福韦治疗3个月,一天两次,不改变患者的免疫抑制治疗方案。在这治疗的3个月内,患者的脚部病变逐渐消失(图B)。最终患者可毫不费力的行走,生活质量也得到提高。
【7】降主动脉内出现多个可移动的血栓
患者女性,85岁,存在原发性血小板增多症、冠状动脉疾病和静脉血栓栓塞病史,因出现腹痛、发烧、呕吐、腹泻而就诊。
体格检查显示下腹部柔软且有压痛。生化检查结果显示,白细胞计数为11800每立方毫米(参考范围,3400-8200),D-二聚体水平为6.7毫克每升(参考范围<0.5),血小板计数为562000个每立方毫米(参考范围,150000-360000),乳酸水平为0.8毫摩尔每升(参考范围,0.5-2.2)。
腹部CT和门控主动脉磁共振成像显示,主动脉内存在4个血栓(箭头所示),贴附在降主动脉壁上,随着心动周期而同步移动。同时还可发现小肠系膜水肿和脾多发梗死。由于可能出现肠系膜缺血,因而进行剖腹探查,但是并没有发现缺血肠管。
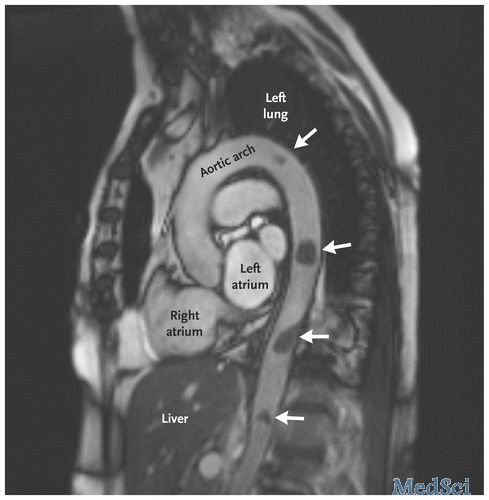
主动脉内出现可移动的血栓是非常罕见的,其发生的机制可能是动脉粥样硬化斑块顶部血栓形成。治疗开始给予抗凝治疗,重复成像显示血栓体积缩小。但是不幸的是,患者出现念珠菌血症,在出现症状后的1个月患者死亡。
【8】硬皮病
患者男性,31岁,因渐进性呼吸短促和皮肤外貌表现8个月而就诊于急诊科。
体格检查显示,皮肤色素脱失区域位于毛囊周围区域,色素沉着部位位于血管表面的皮肤部位(如下图所示)。
前臂活组织检查显示透明样化胶原,符合硬皮病的诊断。真皮乳头层可发现色素减退和噬黑素细胞。盐和胡椒样皮肤改变呈现白癜风样色素脱失。毛囊的毛细血管网仍可合成黑色素,并有色素沉着。患者最初的肺部症状表现是由于间质性肺病所致。皮肤与肺部的症状符合硬皮病的诊断。
给予患者麦考酚酸莫酯和泼尼松治疗其皮肤及肺部症状,患者出现部分反应,肺部症状仍然存在。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了
0
henhao
51
谢谢分享
89
学习谢谢分享
64
学习的
95
感谢分享
76
学习
41