JAHA:DPP-4抑制剂阿拉格列丁能够抑制颅内动脉瘤的形成
2017-06-21 MedSci MedSci原创
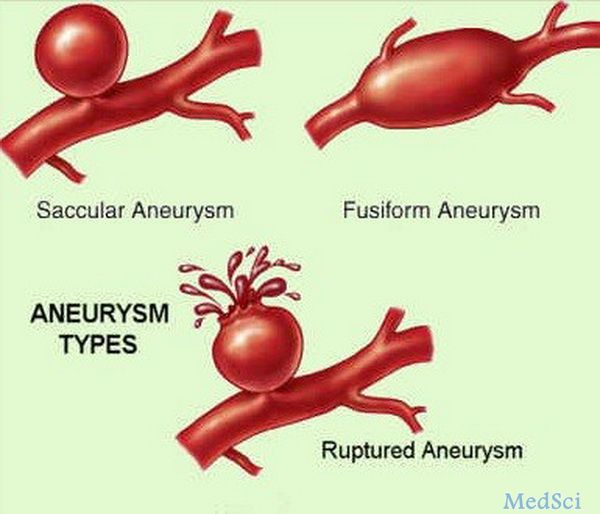
慢性炎症在颅内动脉瘤的病理发生过程中起到关键作用。二肽基肽酶-4(DPP-4)抑制剂有抗炎症作用,包括阻止巨噬细胞浸润等。本次研究的主要目的是利用大鼠动脉瘤模型探索DPP-4抑制剂阿拉格列丁是否有抑制动脉瘤形成的作用。
慢性炎症在颅内动脉瘤的病理发生过程中起到关键作用。二肽基肽酶-4(DPP-4)抑制剂有抗炎症作用,包括阻止巨噬细胞浸润等。本次研究的主要目的是利用大鼠动脉瘤模型探索DPP-4抑制剂阿拉格列丁是否有抑制动脉瘤形成的作用。
大鼠颅内动脉瘤模型通过外科手术的方法建立,并予以口服300 mg/kg 阿拉格列丁治疗。研究者对动脉瘤随时间的形态学参数及其局部炎症反应进行测量评估。为了进一步探索其分子机制,采用了脂多糖处理的RAW264.7巨噬细胞进行研究。在阿拉格列丁处理组,建模后2-4周大鼠的动脉瘤有明显减小。阿拉格列丁在动脉瘤的形成中有抑制巨噬细胞累积的作用,减少了单核细胞趋化蛋白-1(MCP-1)的表达,并且抑制了p65的磷酸化。在脂多糖刺激的RAW264.7细胞中,阿拉格列丁能明显减少肿瘤坏死因子α、MCP-1和IL-6的表达。此外,阿拉格列丁能激活细胞外信号调节激酶-5(ERK-5),该因子介导他汀类药物的抗炎症作用。ERK5抑制剂能够阻遏阿拉格列丁抑制MCP-1和IL-6的表达,并且能够抵消对p65磷酸化的抑制作用。
DPP-4抑制剂阿拉格列丁能够通过抗炎症作用抑制颅内动脉瘤的形成。
原始出处:
Taichi I et al.Dipeptidyl Peptidase‐4 Inhibitor Anagliptin Prevents Intracranial Aneurysm Growth by Suppressing Macrophage Infiltration and Activation.JAHA.2017 June.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
58
#DPP-4抑制#
63
#AHA#
63
#DPP-4抑制剂#
67
#DPP-4#
55
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
75