常用下肢骨折骨科鉴别诊断
2015-01-15 医学界骨科频道 网络
股骨颈骨折 1、股骨转子间骨折 受伤机制与本病相似,但患者年龄常更大,局部肿胀明显,压痛点在股骨为粗隆部,皮肤一般可见瘀斑;X线片可助鉴别。 2、髋关节后脱位 常见于青壮年,有强大暴力损伤史;患肢弹性固定于屈髋、屈膝、内收、内旋位,在臀后可扪及脱出的股骨头;X线片可鉴别。 股骨转子间骨折 1、股骨颈骨折 受伤机制与本病类似,但年龄琦对较小,局部肿胀及痕斑不甚明显,压
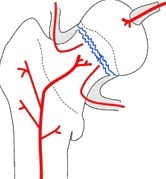
股骨颈骨折
1、股骨转子间骨折 受伤机制与本病相似,但患者年龄常更大,局部肿胀明显,压痛点在股骨为粗隆部,皮肤一般可见瘀斑;X线片可助鉴别。
2、髋关节后脱位 常见于青壮年,有强大暴力损伤史;患肢弹性固定于屈髋、屈膝、内收、内旋位,在臀后可扪及脱出的股骨头;X线片可鉴别。
股骨转子间骨折
1、股骨颈骨折 受伤机制与本病类似,但年龄琦对较小,局部肿胀及痕斑不甚明显,压痛点在腹股沟中点;X线摄线可助鉴别。
2、髋关节后脱位 常见于青壮年,有强大暴力损伤史;患肢弹性固定于屈髋、屈膝、内收、内旋位,在臀后可扪及脱出的股骨头;X线片可鉴别。
3、股骨干上1/3骨折 青壮年及儿童多见,有明显外伤史;局部压痛敏锐,出现短缩、成角或旋转畸形,可扣及骨擦感和异常活动;X线片示股骨干骨折,
股骨干骨折
1、股骨转子间骨折 常见于老年人,压痛点在股骨大转子;X线片可鉴别,
2、股骨髁上骨折 股骨髁上处压痛敏锐、骨擦感,和异常活动;X线片示髁上骨折。
股骨髁上骨折
1、膝关节脱位 暴力强大,疼痛剧烈,肿胀严重,膝关节弹性固定在某一位置上,无骨擦音;X线摄片鉴别。
2、髌骨骨折 膝前髌骨部位压痛,有移位骨折可扪及骨折分离所致的凹陷,伸膝功能障碍;X线摄片可协助鉴别。
股骨髁间骨折
股骨髁上骨折 骨折发生在腓肠肌起点以上2厘米-4厘米范围内,短缩、成角、旋转畸形,可有异常活动;X线摄片骨折线不进入关节.
髌骨骨折
1、副髌骨骨折 局部无明显压痛,伸膝无明显受限;X线片见骨块边缘整齐、光滑,多对称存在,多发生在髌骨的外上角.
2、股骨髁部及髁上骨折 受伤暴力较大;压痛点在股骨髁部及髁上,可出现畸形,有骨擦音;X线摄片可鉴别。
3、胫骨平台骨折 压痛点在胫骨内名外侧平台,髌骨前面摸不到裂隙;X线摄片鉴别。
胫骨髁骨折
1、股骨髁部骨折 暴力强大,压痛点在股骨裸髁部,X线片示股骨髁骨折。
2、髌骨骨折 髌骨部压痛、裂隙,膝不能伸直,X线片示髌骨骨折。
踝部骨折脱位
1.距骨骨折脱位 多由高处跌下所致;压痛点在距骨,X线片可协助鉴别.
2.踝部韧带损伤 多由踝关节所扭伤所致;肿痛,压痛点在内踝下方或外踝的前下或下方;无内擦音和畸形;X线摄片可排除骨折。
距骨骨折
1、踝部骨折 压痛点在内或外踝,有畸形和骨擦音;x线摄片可协助诊断.
2、跟骨骨折 高处跌下所致.足跟部有瘀斑、压痛;骨折移位严重出现扁平足,后跟增宽;x线摄片可鉴别。
3、先天性距骨后三角骨 无明显外伤史,多由扭伤踝部照片时发现;照双侧X线片对比多为对称性,三角骨与距骨后侧紧密相连,骨片界线清晰、光滑。
足舟骨骨折
1、距骨骨折 多由高处跌下所致,压痛点在距骨,X线摄片鉴别。
2、副舟骨 为对称性,与舟骨体连接平面齐整光滑,局部无压痛。
趾骨骨折
趾拓或趾间关节脱位 足趾弹性固定在某一位置,无骨擦音;X线片可鉴别。
跖骨骨折
1.第五跖骨基底骨骺未闭:小儿受到外伤后出现肿胀、疼痛,不能行走,摄片发现有骨骺未闭合时,与健侧对比,以便明确诊断。
2.腓骨长肌腱籽骨:受伤后同样有肿胀、疼痛,但肿胀、疼痛不明显,骨片光滑、规则,双侧均有。
躯干骨骨折-胸骨骨折
胸壁软组织挫伤 无畸形及骨擦感,胸廓挤压征阴性,X线片无骨折征。
肋骨骨折
胸壁软组织挫伤 伤后初期疼痛逐渐加重,无明显固定的压痛点;且不能触及骨擦感,胸廓挤压征阴性;X性摄片可资鉴别。
脊柱骨盆骨折 -脊髓损伤
1、脊椎前角灰质炎 多见于小儿;否认外伤史,一般都有高热史;往往出现的是部分肌群的瘫疾;X线摄片无骨折脱位。
2、脊柱结核 无明显外伤史;有全身结核中毒症状、冷脓肿、瘘道;X线片可鉴别。
3、脊柱脊髓肿瘤 一般无外伤史;神经症状逐渐加重,疼痛晚上较甚;X线摄片及CT扫描可协助鉴别。
颈椎骨折脱位
颈椎病 多见于老年人,无明显外伤史或伤前已有症状;诉双手麻木无力或头晕外,常不合并截瘫,部分截瘫患者常为渐进性;X线摄片可明确鉴别。
胸腰椎骨折脱位
急生腰扭伤 多为腰部用力过度或体位不正闪扭所致;无纵向叩击痛和后凸畸形;X线摄片检查可明确诊断。
骨盆骨折
股骨颈或股骨粗隆间骨折 多见于老年人;患肢常有短缩外旋畸形,大粗隆上移;X线片可鉴别.
尾椎骨折脱位
钩状尾骨骨折 无压痛,肛门指检无明显活动或仅有轻度活动感。
腰椎间盘突出症
1、腰椎后关节紊乱 相邻椎体的上下关节突构成腰椎后关节,为滑膜关节,有神经分布。当后关节上、下关节突的关系不正常时,急性期可因滑膜嵌顿产生疼痛,慢性病例可产生后关节创伤性关节炎,出现腰痛。此种疼痛多发生于棘突旁1.5厘米处,可有向同侧臀部或大腿后的放射痛,易与腰椎间盘突出症相混。该病的放射痛一般不超过膝关节,且不伴有感觉、肌力减退及反射消失等神经根受损之体征。对鉴别困难的病例,可在病变的小关节突附近注射2%普鲁卡因5毫升,如症状消失,则可排除腰椎间盘突出症。
2、腰椎管狭窄症 间歇性跛行是最突出的症状,患者自诉步行一段距离后,下肢酸困、麻木、无力,必须蹲下休息后方能继续行走。骑自行车可无症状。患者主诉多而体征少,也是重要特点。少数患者有根性神经损伤的表现。严重的中央型狭窄可出现大小便失禁,脊髓碘油造影和CT扫描等特殊检查可进一步确诊。
3、腰椎结核 早期局限性腰椎结核可刺激邻近的神经根,造成腰痛及下肢放射痛。腰椎结核有结核病的全身反应,腰痛较剧,X线片上可见椎体或椎弓根的破坏。CT扫描对X线片不能显示的椎体早期局限性结核病灶有独特作用。
4、椎体转移瘤 疼痛加剧,夜间加重,患者体质衰弱,可查到原发肿瘤。X线平片可见椎体溶骨性破坏。
5、脊膜瘤及马尾神经瘤 为慢性进行性疾患,无间歇好转或自愈现象,常有大小便失禁。脑脊液蛋白增高,奎氏试验显示梗阻。脊髓造影检查可明确诊断。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错,赞一个
171
值得关注
174
这篇文章有一定深度
188
是一篇不错的文章
148
患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施
154
?学习了
129
#鉴别诊断#
92
哈哈,收藏了
147