ST段神奇回落,这是哪路心梗?要立即置入支架么?
2019-02-18 武德崴 医学界心血管频道
你是否曾在值班时遇到这样的情况,患者因胸痛入院,ST段抬高,心肌酶阳性,诊断ST段抬高型心梗(STEMI)确切无疑。但是在急诊经皮冠脉介入治疗(PCI)的准备过程中,患者ST段奇迹般回落,胸痛症状也基本消失,下一步这个患者到底做不做急诊PCI?
你是否曾在值班时遇到这样的情况,患者因胸痛入院,ST段抬高,心肌酶阳性,诊断ST段抬高型心梗(STEMI)确切无疑。但是在急诊经皮冠脉介入治疗(PCI)的准备过程中,患者ST段奇迹般回落,胸痛症状也基本消失,下一步这个患者到底做不做急诊PCI?
血运重建前ST段神奇回落,这是哪路心梗?
ST段在血运重建前完全回落,这种情况称为短暂ST抬高型心肌梗死(Transient STEMI,TSTEMI)。TSTEMI并不罕见,据既往的观察性研究,4%-24%的STEMI患者表现为TSTEMI。在临床中,我们也经常遇到这样的患者。
然而,指南从未对TSTEMI患者的治疗做过推荐。到底应该依照STEMI进行即刻血运重建,还是参考非ST段抬高型心梗(NSTEMI),根据GRACE评分进行延迟血运重建,很多时候,我们仅能依靠术者的经验和精力做出决定,缺乏可靠的循证医学证据。
近期在《欧洲心脏杂志(European Heart Journal)》发表的TRANSIENT研究对这一问题进行了探讨。
即刻PCI vs 延迟PCI,孰优孰劣?
TRANSIENT研究是一项多中心随机对照试验,入选患者符合以下条件:
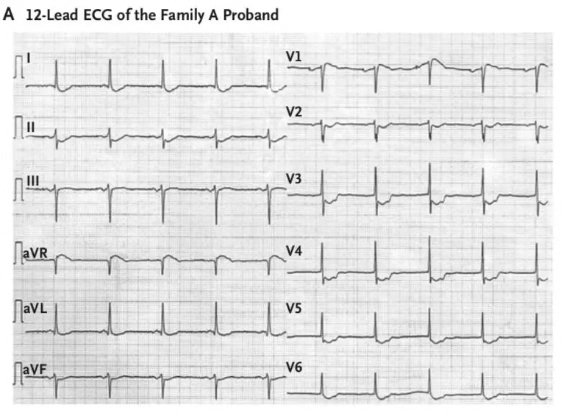
入院前出现急性心肌梗死的临床症状,同时伴有心电图2个以上相邻导联的ST段抬高;
无论院前是否接受过治疗(溶栓除外),入院时症状已完全缓解,ST段完全回落。
研究共入选142例患者,随机分为即刻干预组和延迟干预组,即刻干预组即刻接受造影检查(中位时间0.3h),延迟干预组根据GRACE评分进行延迟造影检查(>140分24小时内进行,≤140分72小时内进行,中位时间22.7h)。
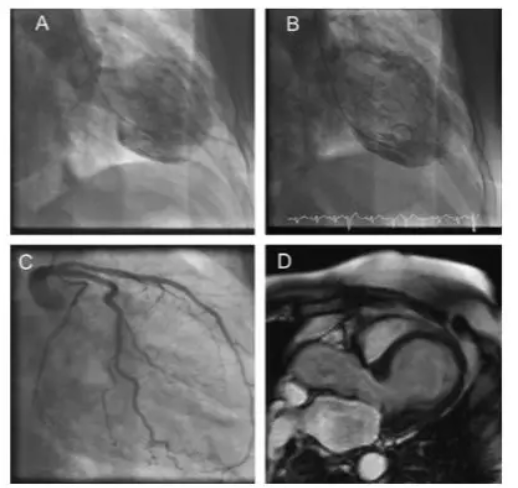
研究的首要终点是发病第4天心脏磁共振检查测量的梗死面积,次要终点是肌酸激酶同工酶(CK-MB)或肌钙蛋白I(TnI)的曲线下面积以及心脏磁共振测量的左室射血分数,同时评估了两种治疗方式下30天的主要不良心血管事件(MACE)发生率。
结果表明,两组患者的平均梗死面积无显着差异(即刻组vs延迟组,1.3%vs 1.5%,P=0.48),30天的MACE无显着差异(即刻组vs延迟组,2.9%vs2.8%,P=1.00)。
不过,延迟组中有4例患者因出现胸痛复发而接受了即刻PCI术。该研究表明,TSTEMI患者即刻PCI治疗和延迟PCI治疗相比,在梗死面积和短期预后方面并未见到显着差异。
陌生不要紧,记住这3个要点!
TRANSIENT研究是第一项评估TSTEMI患者治疗时机的随机对照试验。既往有过类似主题的研究,如ELISA-3试验的事后分析和一些观察性研究也提示类似的结论。这些研究让我们对TSTEMI有了更加深入的认识。
1.TSTEMI是一种相对低危的心肌梗死
在ST段持续抬高的心肌梗死患者中,心脏MR测定的梗死面积多在10%左右,而TSTEMI的梗死范围仅有1%左右;30天3%左右的MACE事件发生率也低于常规的STEMI患者(10%左右)。
因此,大多数TSTEMI的缺血风险远低于常规的STEMI患者。不过,仍有患者在症状缓解,ST段回落后出现症状复发,ST段再次抬高,此时应考虑再梗死的可能性,虽然并无正式的研究数据评估这类患者的预后,但是根据临床经验还是应当将这中情况归为高危患者,在本研究中同样有4例延迟PCI组患者因ST段的再次抬高而接受了即刻PCI治疗。
2.血流是否再通是PCI时机的重要参考
即刻PCI治疗对于缺血高危患者可以迅速开通闭塞血管,挽救梗死心肌。同时也存在诸多风险,急性期患者血栓负荷较重,早期的机械干预可能会导致微血栓堵塞微血管,造成无复流;同时,机械刺激也可能导致新发斑块破裂和新的血栓事件。
延迟PCI可以通过前期的药物治疗稳定破裂斑块,减轻血栓负荷,降低PCI过程中无复流的发生率。因此,对于血流再通的STEMI患者,可以考虑进行延迟PCI治疗。
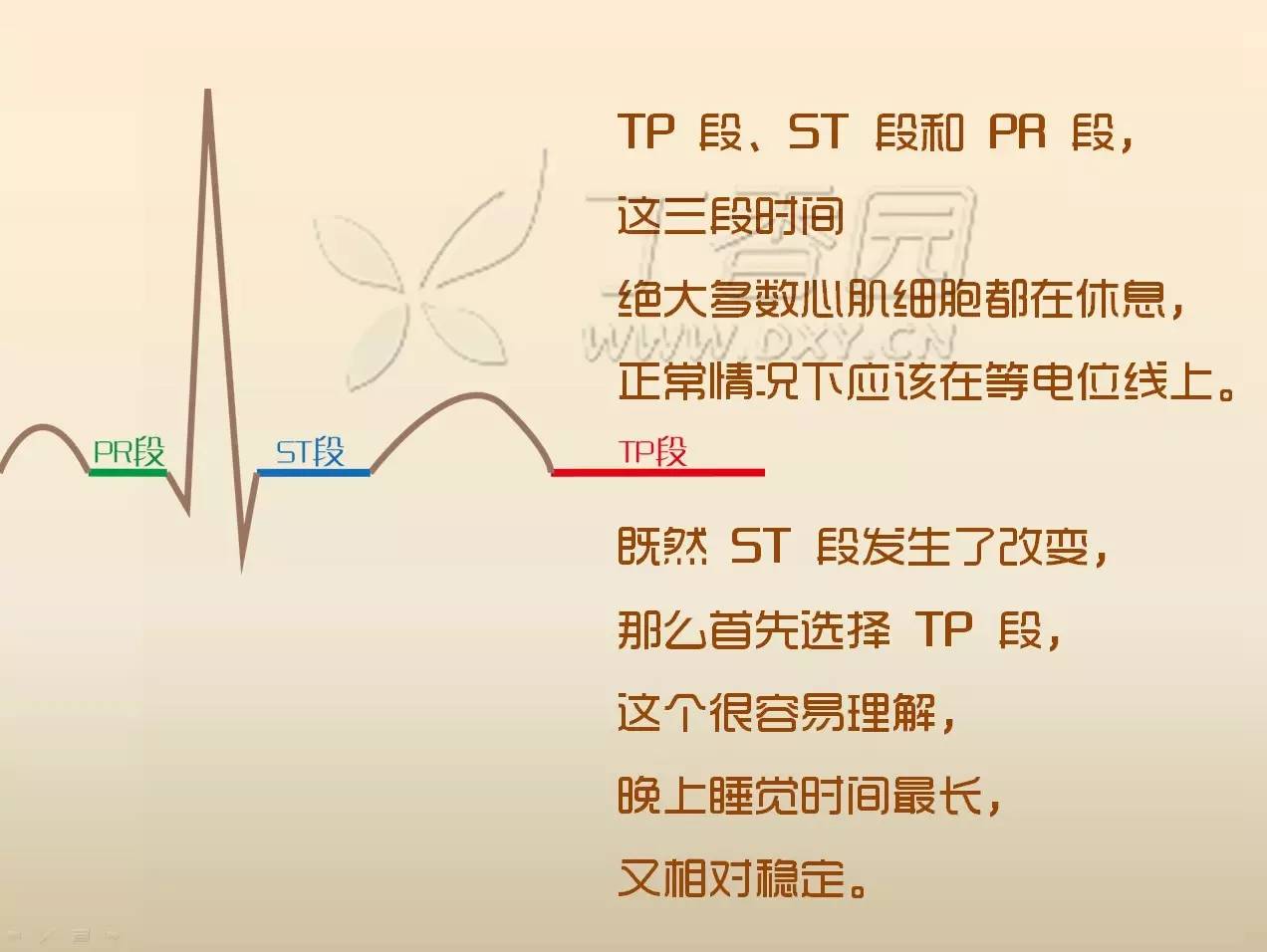
3.通过症状缓解和ST段回落判断血管是否再通
在所有入选患者中,除1例即刻PCI组患者以及2例ST段再次抬高的患者外,其他所有患者均达到TIMI2级以上血流,并有超过90%的患者达到TIMI3级血流。同时,出现ST段再次抬高是血管再次闭塞的重要体现,4例患者中有2例出现了TIMI0-1级血流。因此,对于STEMI患者,心电图的动态观察和症状的评估对指导其预后非常重要。
结语
TRANSIENT研究可以为TSTEMI患者的治疗提供重要的参考:对于ST段完全回落,症状完全缓解的患者,可以依照NSTEMI的处理方式决定治疗时机,行延迟造影检查,同时加强抗栓治疗和稳定斑块治疗。若等待过程中出现ST段再次抬高或胸痛再发,则应参照STEMI,行即刻PCI治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ST段#
86
好文章,点赞啦!认真学习,谢谢分享给广大同好!
135
心肌梗塞的诊断
123
很好的学习机会
101
学习学习学习学习
103