Am J Gastroenterol:相对肾上腺皮质功不全是失代偿期肝硬化患儿发生并发症的危险因素!
2021-09-11 Nebula MedSci原创
相对肾上腺皮质功不全 (RAI) 是短期随访过程中小儿肝硬化并发症发生的危险因素
相对肾上腺皮质功能不全 (RAI) 与肝硬化成人患者的不良预后相关。但迄今为止,还没有关于 RAI 与肝硬化儿童患者预后的相关性研究。本研究旨在前瞻性地探索 RAI 失代偿期肝硬化患儿中的发生率和对患儿临床预后的影响。
在第 1 天和第 21 天,对血流动力学稳定的失代偿期肝硬化患儿进行血清基础皮质醇和峰值皮质醇(静脉注射 1 μg 二十四肽促皮质素 30 分钟后)取样。RAI 诊断标准:皮质醇峰值 <500 nmol/L。血清细胞因子(白细胞介素 6 和肿瘤坏死因子 α)和脂质谱与 RAI 相关。随访 180 天,观察并发症的发生情况和患儿的生存预后。根据已确定的风险因素,推导出预后模型,并与儿科终末期肝病 (PELD) 和 Child-Turcotte-Pugh 评分进行比较。
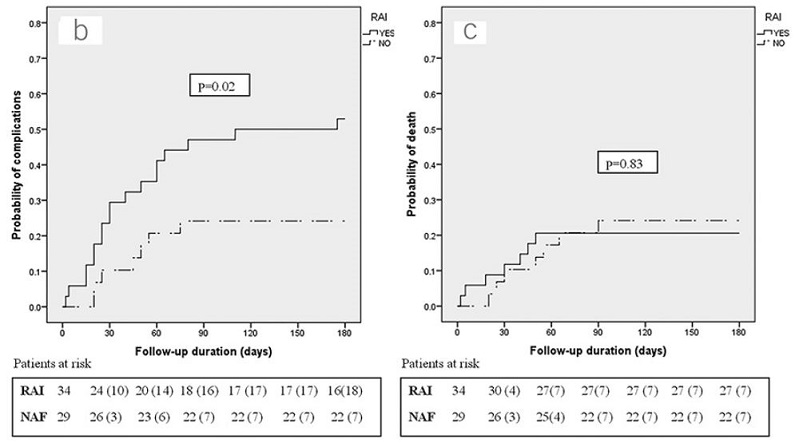
有无RAI的患儿的并发症发生率和死亡率
共招募了 63 位患儿(年龄 128 ± 48 个月,男童占 78%)。在基线和第 21 天时,RAI 的发生率分别是 54% 和 61%。在 RAI 组和肾上腺功能正常组之间的细胞因子和血清脂质水平未见明显差异。与肾上腺功能正常组相比,基线时就存在 RAI(D1-RAI)的患儿在随访过程时并发症的发生率更高(53% vs 24%,p=0.02)。PELD 评分和 D1-RAI 都是随访过程中发生并发症的独立预测因素(风险比[OR]分别是 1.08 [p<0.01] 和 3.19 [p=0.01])。
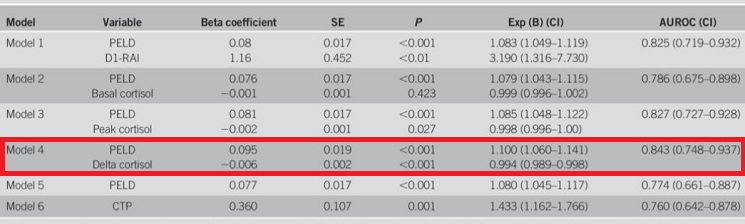
不同模型对随访并发症的预测评分
PELD-delta 皮质醇模型(曲线下面积 0.84,p<0.001; 敏感性 92%, 特异性 60%)比单纯的 PELD 或 Child-Turcotte-Pugh 评分可更好地预测并发症的发病率。
综上所述,相对肾上腺皮质功不全 (RAI) 是短期随访过程中小儿肝硬化并发症发生的危险因素。PELD-delta 皮质醇评分是一种很有前景的预测随访并发症风险的预后模型。
原始出处:
Tripathi Parijat Ram,Sen Sarma Moinak,Yachha Surender Kumar et al. Relative Adrenal Insufficiency in Decompensated Cirrhotic Children: Does It Affect Outcome?[J] .Am J Gastroenterol, 2021, https://doi.org/10.14309/ajg.0000000000001486
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AST#
29
#肾上腺#
41
#GAS#
35
#并发#
34
#失代偿期肝硬化#
45
#Gastroenterol#
30
谢谢!最新的信息读起来就是收获大
0
谢谢!最新的信息读起来就是收获大
43