头颈部侵袭性纤维瘤病1例
2019-08-21 李正强 刘曙光 口腔疾病防治
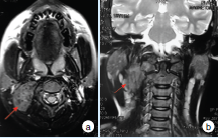
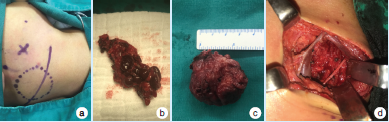
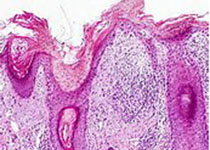
患者,男性,13岁,主诉因“右颈部无痛性肿物半年余”入院。入院查体:右侧颈上部皮肤稍隆起,皮温色泽正常,可触及一大小约3.5 cm×2.5 cm×3.0 cm肿物,前界位于胸锁乳突肌前缘前2.5 cm处,后界位于胸锁乳突肌前缘后1.0 cm处,上界达乳突,下界位于下颌下缘所在平面,表面光滑,活动度差,质硬,无触痛。入院前B超检查提示:右侧颈部皮下实质团块,待排良性间叶组织来源肿瘤。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
80
#侵袭性#
0
#纤维瘤#
55
#头颈部#
70
#颈部#
0
#纤维瘤病#
72