Stem Cell Rep:人脑实验力证:超声波大大助力老年痴呆治疗,血脑屏障不再是阻碍!
2020-04-12 Paris 转化医学网
近日,一项新的研究探索了超声波治疗对阿尔茨海默病患者的潜在益处。研究人员发现,使用聚焦超声结合微泡治疗,可以在由人类内皮细胞形成的血脑屏障中创造开口,从而向阿尔茨海默病患者递送靶向药物,新型超声治疗方
近日,一项新的研究探索了超声波治疗对阿尔茨海默病患者的潜在益处。研究人员发现,使用聚焦超声结合微泡治疗,可以在由人类内皮细胞形成的血脑屏障中创造开口,从而向阿尔茨海默病患者递送靶向药物,新型超声治疗方法有望变革阿尔茨海默病的治疗,从根本上改变人们对其治疗的传统理解。该研究是首次在小鼠和其他动物模型的基础上,对人类阿尔茨海默病患者脑细胞的研究技术进行了研究。相关研究以“Altered Brain Endothelial Cell Phenotype from a Familial Alzheimer Mutation and Its Potential Implications for Amyloid Clearance and Drug Delivery”为题在线发表在《Stem Cell Reports》杂志上。
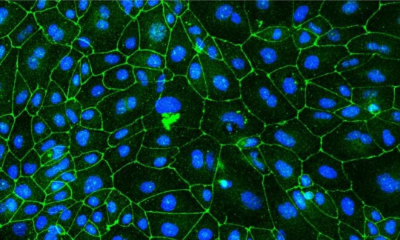
阿尔茨海默病是痴呆症中最常见的病因,目前尚无有效的治疗方法。血脑屏障是一个由血管和组织构成的网络,它阻止外来物质进入大脑。血脑屏障对研究治疗方法的科学家提出了挑战,因为它还会阻止潜在的治疗药物到达大脑内部的目标。
有研究表明,利用超声技术可以去除沉积在老年痴呆症患者大脑中导致记忆丧失和认知下降的一种淀粉斑,从而能够帮助患者恢复记忆。在本次研究是建立在之前研究的基础上,通过使用聚焦超声和微泡治疗,研究人员发现,这可以削弱血脑屏障细胞之间的联系,从而让脑组织吸收药物治疗成为可能。在AD小鼠模型中,应用瞬时开放血脑屏障的聚焦超声(FUS),发现AD细胞对3-5 kDa右旋糖酐的通透性改变,AD-iBECs中淀粉样蛋白-β(Aβ)肽的通透性改变。微泡会因应超声波而振动以暂时性地开放血脑屏障。用聚焦超声和微泡来穿透人脑的方法迄今已在猴子中做过测试。这提供了人类衍生的BBB的体外模型作为一个有价值的工具,以了解其在疾病背景下的作用和特性,并可能对药物的传递产生影响。
他们将脂质微泡注入细胞,然后用超声波瞄准该区域,导致细胞扩张和收缩,破坏细胞之间的连接,打开血脑屏障。他们发现,在不损伤脑组织的情况下,超声波在75%的小鼠中几乎完全清除了斑块。与未经治疗的小鼠相比,接受过治疗的小鼠显示了记忆力的改善,它们在三种记忆测试中的表现都更好;这三种记忆测试为Y型-迷宫、新物体识别测试和场所主动回避活动。脑组织分析显示,超声刺激了小胶质细胞(即可吞噬细胞碎片的免疫细胞)摄取更多的β淀粉样蛋白斑块。动物实验顺利进行,随后,研究人员在人脑中进行了下一步的实验验证。
该研究的第一作者、QIMR Berghofer研究员洛塔·奥卡里博士表示,人脑实验发现,超声和微泡疗法对阿尔茨海默病患者脑细胞的持久影响比健康对照组更长。治疗在所有患者的血脑屏障的单层中产生了开口,但健康对照组的脑内皮细胞修复得比老年痴呆症患者的细胞要快,老年痴呆症患者的血脑屏障修复较慢,这表明他们更容易接受药物和治疗,而且脑超声治疗需要根据患者的疾病类型进行不同的调整。
该研究首次探讨了人类患者的血脑屏障细胞如何被破坏,以提高阿尔茨海默病药物治疗的吸收,为阿尔茨海默病的治疗带来了新的曙光。
原始出处:Lotta E. Oikari, Rucha Pandit, Romal Stewart, et al. Altered Brain Endothelial Cell Phenotype from a Familial Alzheimer Mutation and Its Potential Implications for Amyloid Clearance and Drug Delivery, Stem Cell Reports (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
83
#CEL#
66
#超声波#
95
#stem cell#
77
#血脑屏障#
131
#STEM#
72
学习了
117
老年人痴呆何药可用??
97