IBD: 托法替布治疗溃疡性结肠炎疗效的预测因素分析
2022-09-13 xuyihan MedSci原创
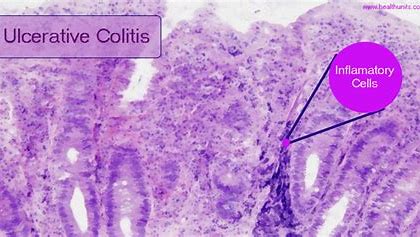
溃疡性结肠炎属于炎症性肠病之一,炎症性肠病主要分为克罗恩病和溃疡性结肠炎。溃疡性结肠炎的临床表现为黏液脓血便、腹痛、大便不成形伴随里急后重感,还有大便解不尽的感觉。
溃疡性结肠炎(UC)是结肠相关的一种慢性疾病,其特征是炎症复发和缓解反复交替,就严重程度、病程和对治疗的反应而言,溃疡性结肠炎是一种异质性疾病。UC治疗通常会出现继发性反应丧失,乌司奴单抗、维多珠单抗、托法替布和英夫利昔单抗的随机临床试验报告维持治疗44-54周后治疗反应率丧失高达30%-55%。
因此,需要具有不同作用机制的多种治疗方法。因此,为了更好地表征患者群体、优化治疗并最大限度地减少不良事件 (AE)的发生,需要确定可预测维持治疗反应的因素。找到一种方法来预测对治疗的反应将有助于临床医生更好地评估有不良预后风险和最有可能从特定治疗中受益的患者。托法替尼(Tofacitinib) 是一种口服小分子Janus激酶抑制剂,可以用于治疗UC。本项研究旨在探究接受托法替尼维持治疗的中度至重度活动性 UC 患者持续反应和缓解的预测因子。
研究人员将具有临床反应的UC患者重新随机分配接受托法替尼5或10mg每天两次或安慰剂治疗。研究人员同时在基线特征按第52周疗效终点(缓解、持续缓解、临床反应、持续临床反应)进行分层。最后使用逻辑回归分析评估基线特征和疗效终点之间的关联。

研究结果显示:487名UC患者中有170名(34.9%)患者在第52周时缓解。在多变量建模中,基线时的内窥镜评分(2 vs 3;优势比 [OR],1.60;95% 置信区间 [CI ],1.06-2.44]),Mayo评分(<2 vs ≥2;OR,1.92;95% CI,1.27-2.90)和年龄(每 10 年;OR,1.19;95% CI,1.02-1.39 )与第52周时更高的缓解几率相关。口服皮质类固醇的使用(OR,0.63;95% CI,0.42-0.96)和C反应蛋白(OR, 0.94; 95% CI, 0.89-0.99) 与第52周疾病缓解的可能性降低相关。
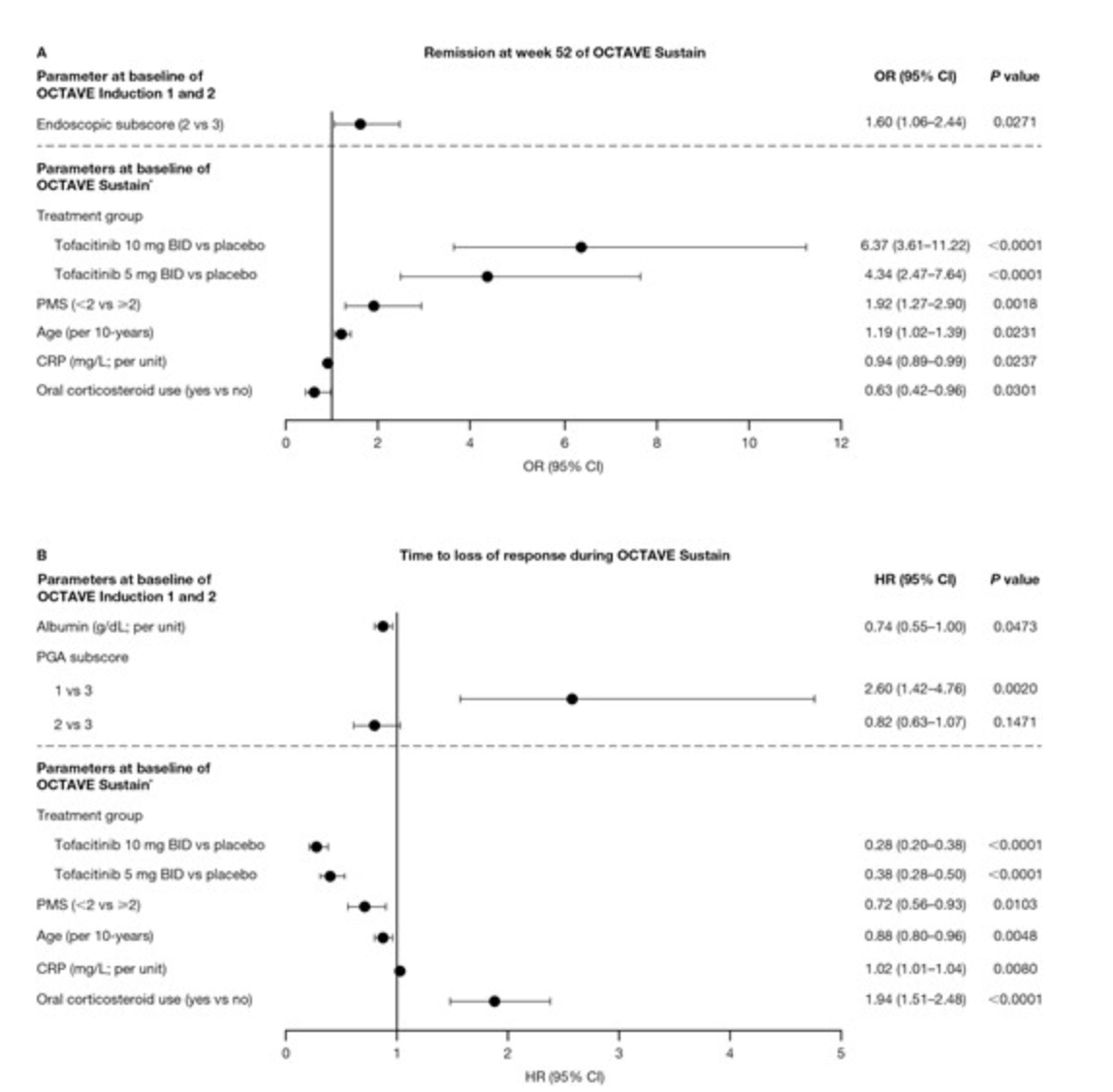
本项研究证实托法替布诱导治疗8周后临床改善更大的患者更有可能维持托法替尼的反应或维持疾病缓解,无论维持期间接受的剂量如何,初期应答非常重要。
原始出处:
William J Sandborn. et al. Predictors of Sustained Response With Tofacitinib Therapy in Patients With Ulcerative Colitis. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#溃疡性#
72
学习
79
#IBD#
87
#预测因素#
98
#治疗溃疡性结肠炎#
85