Nature:美国南加州大学学者发表药物靶标AT2R结构研究成果
2017-04-10 佚名 生物帮
摘要:2017年4月5日,国际学术权威刊物自然出版集团《Nature》杂志在线发表了美国南加州大学VadimCherezov教授、VsevolodKatritch教授和浙江大学药学院张海涛课题组合作的一篇研究论文2017年4月5日,国际学术权威刊物自然出版集团《Nature》杂志在线发表了美国南加州大学Vadim Cherezov教授、Vsevolod Katritch教授和浙江大学药学院张海涛课
摘要:2017年4月5日,国际学术权威刊物自然出版集团《Nature》杂志在线发表了美国南加州大学VadimCherezov教授、VsevolodKatritch教授和浙江大学药学院张海涛课题组合作的一篇研究论文
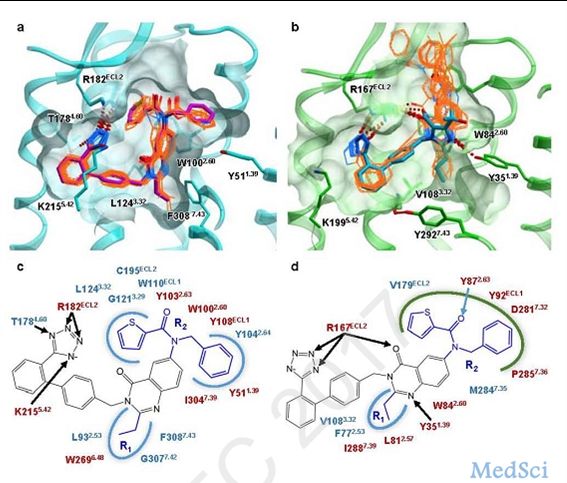
2017年4月5日,国际学术权威刊物自然出版集团《Nature》杂志在线发表了美国南加州大学Vadim Cherezov教授、Vsevolod Katritch教授和浙江大学药学院张海涛课题组合作的一篇研究论文《血管紧张素II受体的选择性和多样性的结构基础》(Structural Basis for Selectivity and Diversity in Angiotensin II Receptors)。研究应用最新的自由电子激光技术(XFEL)和同步辐射,首次解析了AT2R与两种药物先导化合物的复合物晶体三维结构,其中一种是AT2R选择性配体,另一种是AT1R/AT2R双靶点配体,并通过一系列构效关系研究、分子对接、分子动力学和突变实验,系统阐明了不同亚型血管紧张素II受体的配体选择性和功能多样性的结构基础,从而为基于结构的AT1R/AT2R靶向药物研究提供了关键信息。张海涛研究员为该论文的第一作者,Vadim Cherezov教授和Vsevolod Katritch教授是论文的通讯作者。
在人体中,内源激素血管紧张素II的效应由AT1R和AT2R两种G蛋白偶联受体(GPCR)进行调控。AT1R主要负责调节血压,其阻断剂在临床上被广泛用作降血压药物;AT2R与血压调控、神经生长、疼痛控制和心肌再生相关,靶向AT2R的药物可以改善心血管功能、缓解神经性疼痛等。张海涛研究员的前期研究成果首次解析了AT1R与两种沙坦类降血压药物的复合物晶体三维结构(Zhang, et al. Cell.2015 May 7;161(4):833-44. Zhang, et al. J Biol Chem. 2015 Dec 4;290(49):29127-39.),现在又进一步解析了AT2R与两种药物先导化合物的复合物晶体三维结构。该研究发现,AT1R和AT2R在跨膜区和配体结合区存在显著的结构差异,提示AT2R处于类激活的构象,而且AT2R羧基末端的螺旋VIII与之前报道的其它GPCR结构也截然不同,它结合在AT2R胞内区G蛋白和β阻遏蛋白的位点,并与螺旋V和VI相互作用。分子动力学研究表明,螺旋VIII稳定了AT2R的类激活态构象,同时阻碍了G蛋白和β阻遏蛋白的偶联,该重要发现为研究AT2R的生理学和病生理学功能提供了重要的结构信息。
Nature同时在线发表了英国剑桥MRC分子生物学实验室的Christopher G. Tate教授对本论文的评论文章《结构生物学:一种自抑制的受体》(Structural biology: A receptor that might block itself),评论文章认为AT2R的结构揭示了一种潜在的自抑制机制,因此该晶体结构非常富有启发性(The structure of the angiotensin II type 2 receptor reveals a potential mode of self-blocking action. Zhang and colleagues' crystal structure of AT2R is therefore highly illuminating. )。AT2R非同寻常的药理学性质已经困扰人们很多年,该结构第一次提供了支持这个非同寻常行为的见解。The unusual pharmacology of AT2R has been a puzzle for many years. Zhang and colleagues' structure provides the first insight into what might underpin this unusual behaviour. )
原始出处:
Haitao Zhang, Gye Won Han, Alexander Batyuk, et al. Structural basis for selectivity and diversity in angiotensin II receptors[J]. Nature, 2017.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#研究成果#
70
#Nat#
71
#靶标#
77
#药物靶标#
91
学习中
113