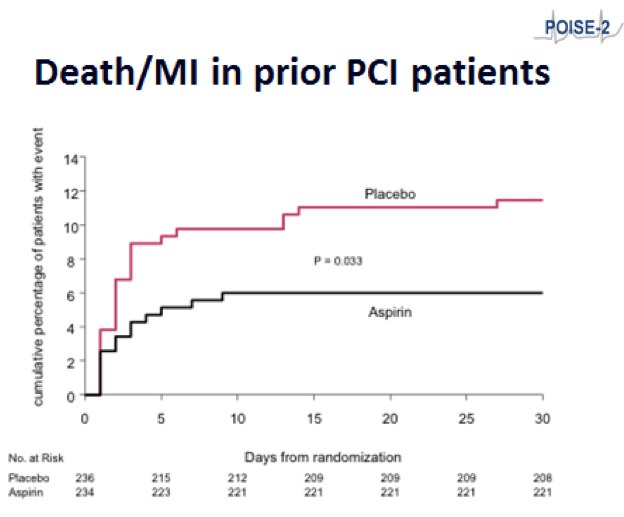
Neurology:低剂量阿司匹林不增加颅内出血风险,反而降低SAH风险
2017-12-10 杨中华 脑血管病及重症文献导读
低剂量阿司匹林广泛应用于缺血性血管事件的二级预防,甚至用于一级预防。随机对照试验或随机对照试验联合队列研究的meta分析把阿司匹林和颅内出血风险增加联系起来,发现二者未达到统计学意义或处于边缘状态。观察性研究的结果更是模棱两可,甚至有研究认为长期服用阿司匹林能够降低蛛网膜出血的风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
144
#低剂量阿司匹林#
149
研究有偏倚还是真实?
187
#SAH#
83
#低剂量#
134