手术技巧:肩关节置换治疗肱骨近端骨折
2014-07-09 佚名 丁香园
肱骨近端骨折(PHFs)约占老年人骨折的4%-10%,发病率仅次于髋关节和桡骨远端骨折。其中约有15%的患者需要手术治疗,包括骨折固定术和肩关节置换术。而术后的临床预后要取决于骨折移位部位和程度、肱盂关节的损伤情况和骨质疏松症等危险因素。 实际上,大部分患者可恢复到肩关节原来的活动能力,但术后并发症率高达40%-60%。肱骨头缺血性坏死(AVN)是最应关注的并发症,因为它可引起慢性疼痛、
肱骨近端骨折(PHFs)约占老年人骨折的4%-10%,发病率仅次于髋关节和桡骨远端骨折。其中约有15%的患者需要手术治疗,包括骨折固定术和肩关节置换术。而术后的临床预后要取决于骨折移位部位和程度、肱盂关节的损伤情况和骨质疏松症等危险因素。
实际上,大部分患者可恢复到肩关节原来的活动能力,但术后并发症率高达40%-60%。肱骨头缺血性坏死(AVN)是最应关注的并发症,因为它可引起慢性疼痛、肢体运动功能障碍和需再次手术治疗。
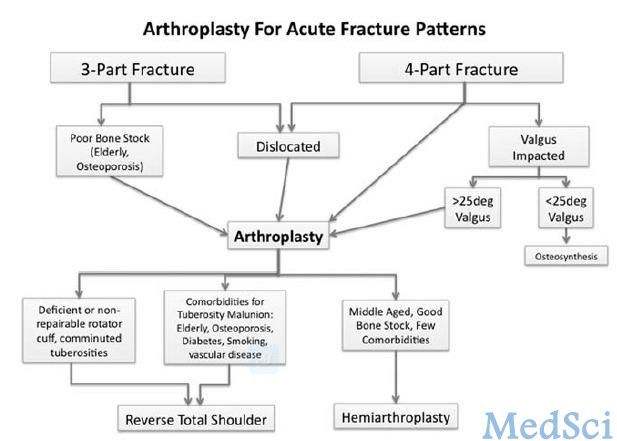
肩关节置换术适用于治疗肱骨粉碎性三部分骨折和大部分四部分骨折,因为这类骨折发生肱骨结节不愈合和肱骨头缺血坏死的风险较高。半肩关节置换术是最常用的手术选择,但是它的疗效受肱骨结节部骨折块愈合情况的影响,所以越来越临床医生倾向于选择反置式肩关节置换术治疗这类骨折。
Grant H.Garcia教授在文章中回顾了肱骨近端骨折的分型,提出了半肩关节置换术和反置式肩关节置换术的手术适应证和禁忌症,文章发表在2013年的Techniques in Orthopaedics上。
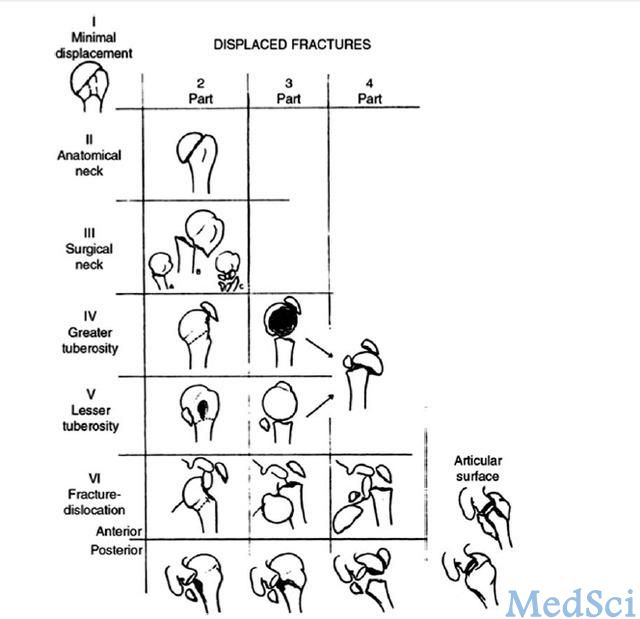
临床上较为常用的肱骨近端骨折分型为Neer分型。根据肱骨四个解剖部位,即小结节、大结节、肱骨头和近端肱骨干,及相互之间移位程度即以移位>1cm(或大结节移位>0.5cm)或成角畸形>45°为移位标准来进行分型(图1)。
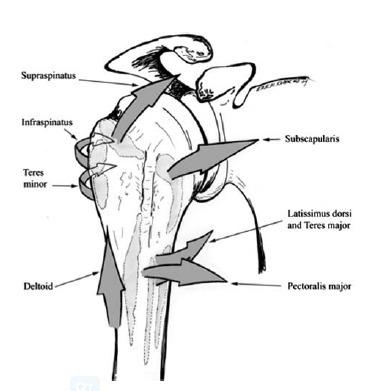
了解肱盂关节的结构对治疗肱骨近端骨折非常重要(图2)。肱骨大结节由于肩袖肌群的作用向后内侧移位,小结节在肩胛下肌的作用下向内侧移位,而肱骨干由于胸大肌的作用向内侧移位和三角肌的作用呈外展。
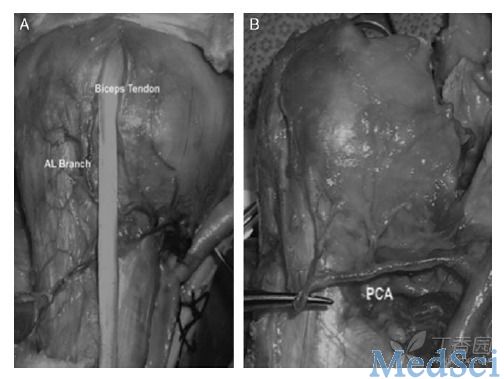
供应肱骨头的动脉有旋肱后动脉、旋肱前动脉及其末梢分支弓形动脉(图3)。它可影响切开复位内固定术和半肩关节置换术治疗肱骨近端骨折的疗效。最新研究指出旋肱前动脉供应肱骨头36%的血液,而剩下的64%是由旋肱后动脉供应。这一发现改变了肱骨近端骨折的治疗方法,并指导临床医生切开复位固定骨折部位。
半肩关节置换术适应证
正确评估肱骨头发生缺血性坏死的危险因素对手术方式的选择至关重要。Boileay教授的研究表明肱骨近端两部分骨折发生肱骨头缺血性坏死的概率<10%,而三部分骨折为10%-25%,因此,大部分采取非手术治疗或切开复位内固定术。而四部分骨折的缺血性坏死概率高达60%,,当同时合并有骨折块移位,则肱骨头发生缺血性坏死的概率为80%-100%。故大多数医生选择半肩关节置换术治疗四部分骨折。
但是,肱骨近端外翻型压缩性四部分骨折因中间软组织无明显损伤,肱骨头发生缺血性坏死的概率只为25%-30%。还有研究指出肱骨近端三部分和四部分骨折的内翻角度>20°应选择半肩关节置换术治疗。
患者的基本情况也影响治疗的效果。如骨质疏松症可影响骨折愈合和导致内固定物的失败,故这类患者应行肩关节置换术。另外,如肩袖肌群损伤将影响患者半肩关节置换术后的患者肩关节的功能恢复。
半肩关节置换术的手术技巧
作者推荐使用改进的“沙滩椅”体位:床头上升至45°,臂下垂位可允许切口延伸。辨认头静脉后,采取胸三角肌入路(deltopectoral approach),分离三角肌和肩峰下区域,辨认出肱二头肌间沟。行Mason-Allen缝合修复肩袖肌群可帮助复位肱骨结节。
肱骨结节间骨折的骨折线常见于结节间沟稍后侧。接着,切除肱骨头,通过内侧和外侧Bennet牵开器暴露肱骨干,在连续扩髓腔后钻孔,就完成髓腔的准备工作。同时,手术医生必须根据上述的解剖标志选出合适的肱骨假体。
然后,在骨折处1.5cm远打两个穿透骨的钻孔,第一条缝线从外面经过其中一个钻孔穿向肱骨近端,可把大结节固定在肱骨假体上,另一条缝线行8字缝合法从前往后把结节与肱骨假体固定在一起。作者推荐使用非骨水泥型假体,但是需考虑到患者的骨质疏松的程度和骨折线的长度。
在假体植入完成前,还需尝试骨折复位,可明确假体的尺寸是否合适和肩关节的稳定性。
假体获得满意的固定后,手术医生需把肱骨结节与假体固定在一起。首先,穿过大结节中间骨折的缝线缠绕假体,纵向的缝线穿过肱骨干远端的钻孔缠绕大结节,穿过大结节顶端和尾部的两条缝线穿过小结节。然后,把大结节牵到假体前面,并固定在肱骨头顶端5cm处,穿过大结节中间缝线和穿过肱骨干远端孔的缝线绑在一起,穿过大结节顶端和尾部的缝线绑在一起,帮助复位肱骨大小结节。从肱骨干远端穿向近端缝线行8字缝合法绑在肱骨结节上。
术后需评估肩关节的稳定性和活动范围,并通过X线平片了解假体和肱骨结节复位情况。
半肩关节置换术的术后并发症如假体松动、肩袖肌群损伤或肱骨结节不愈合,均可影响临床预后。目前,越来越多医生倾向于使用反置式肩关节置换术治疗股骨近端骨折。
反置式肩关节置换术的适应证
目前,反置式肩关节置换术的适应证包括肩袖功能障碍,肱骨大结节骨折不愈合的肱骨近端骨折等。
另外,患者的基本情况可影响肱骨结节的术后愈合情况,如合并有骨质疏松症、粉碎性骨折和女性患者等。完成危险因素评估后,还需了解患者受伤前肩关节的活动功能。如受伤前已患有肱盂关节炎,则应行反置式肩关节置换术。当发生急性肱骨近端骨折或半肩关节置换术失败可选择反置式肩关节置换术。
反置式肩关节置换术的手术技巧
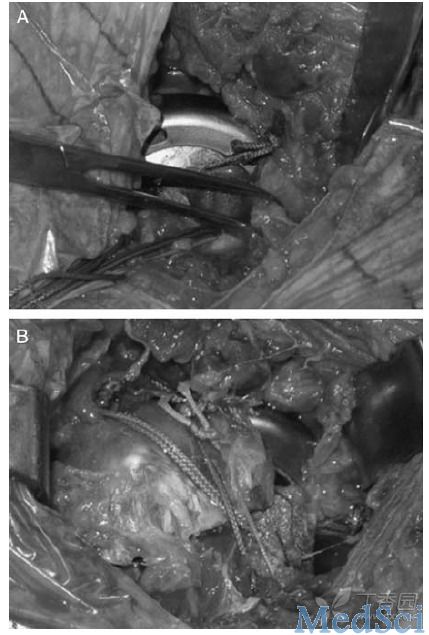
作者认为反置式肩关节置换术的关键是肱骨结节的重建(图4)。患者取Semi-Fowlers位,手臂自由下垂,以便内收和过伸肩时能自由移动。采用标准的胸肌入路,充分暴露术野后,肱骨大小结节用不可吸收粗线在肌腱和骨的交界处标记。
接着,去除肱骨头骨折块,手法扩髓腔以防发生医源性骨折或骨折部位扩大。用牵开器暴露关节盂,扩大关节盂区域,置入基板(baseplate),打入螺钉固定,再置入glenosphere。
然后,在肱二头肌间沟的后外侧和后内侧分别钻2个孔,用不吸收线穿过固定肱骨结节。肱骨假体呈后倾20-30°打入髓腔,根据假体试模位置复位肩关节。测量肩关节活动范围和三角肌张力后,取出假体试模,再置入glenosphere,打入肱骨假体。
接下来就是肱骨结节的重建,穿过结节横行的缝线缠绕肱骨内侧后,在肌肉与肌腱连接处出来再穿过另一个肱骨结节固定。然后,打入肱骨臼假体,肩关节就复位成功。最后,原先穿过肱骨干的纵行缝合穿过肱骨大小结节上侧后打结固定,横行缝线也紧接着打结固定。完成肱骨结节重建后,可通过外展和旋转肩关节确认肱骨结节稳定。
术后康复锻炼
术后用带有外展垫的肩关节吊带固定器至少6周促进肱骨结节愈合。在此期间,鼓励患者行远端肢体的主动功能锻炼,适度的120°以内的被动钟摆运动有助于肩关节功能的恢复。如果术后平片提示肱骨结节愈合和无骨折移位的影像学证据,则鼓励患者在术后6周开始进行肩关节主动功能锻炼。
半肩关节置换术与RTSA的疗效比较
Gallint教授等回顾性研究了肱骨近端复杂性三或四部分骨折患者分别行半肩关节置换术或反置式肩关节置换术治疗的疗效。结果显示RSTA组的肩关节活动功能恢复更好,其中外展和前屈角度分别为91°和97.5°,而半肩关节置换术后组只有60°和53.5°。另外,RSTA组的Costant评分比半肩关节置换组高14分(53比39)。结果表明RSTA组的患者手术肩关节功能恢复更好。
还有研究表明由于两种手术术后患者肱骨结节愈合情况的不确定性,大于70岁的患者行RSTA治疗肱骨近端复杂性三或四部分骨折疗效更好。
Gallint教授的另一研究指出,长期随访证明RSTA术后患者预后更好,但是手术医生在选择手术方式时必须考虑到手术费用与患者的寿命(图5)。
总而言之,作者认为半肩关节置换术适用于治疗肱骨近端骨折复杂性三或四部分骨折,尤其是有肱骨头坏死高风险的或合并有骨质疏松等疾病的患者。但是,患者的愈合与手术医生的水平和患者本身的基本情况密切相关。所以,越来越多医生倾向于使用反置式肩关节置换术。因为他们认为RSTA可以抵消骨质严重疏松、肱骨结节不愈合和肩袖病理性损伤等危险因素。
虽然研究表明RSTA患者术后肩关节功能恢复良好,但是高术后并发症率不可忽视。但目前仍缺少相关的询证医学证据指导作出统一的手术适应证。只能由手术医生根据其丰富的临床经验作出正确手术方式的选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肩关节置换#
94
#置换治疗#
103
#置换#
72
#肩关节#
117
#肱骨#
0
#近端#
86