Front in Immu:烟酸受体与肠道菌群互作参与调控肠道屏障
2018-09-24 撰文 Lee 编辑 紫苏 科研圈
近日,吉林大学动物医学学院研究者联合广东省微生物研究所(华南应用微生物国家重点实验室)研究团队科研人员共同发现,肠道菌群与宿主烟酸受体GPR109A互作、调控肠道屏障,其介导的互作机制对肠道菌群均一性和多样性产生了重要的影响。
近日,吉林大学动物医学学院研究者联合广东省微生物研究所(华南应用微生物国家重点实验室)研究团队科研人员共同发现,肠道菌群与宿主烟酸受体GPR109A互作、调控肠道屏障,其介导的互作机制对肠道菌群均一性和多样性产生了重要的影响。本研究还发现通过粪菌移植可以对实验性败血症的发展起到保护作用。相关成果发表在国际期刊Frontiers in Immunology上(IF:5.511,论文信息见文末)。
在全球强致死性疾病,败血症的发病过程中可能会出现由细菌,病毒或真菌感染导致的炎症反应,进而通过革兰氏阴性菌分泌的脂多糖(LPS)与宿主免疫系统互作诱发系统性炎症反应和器官衰竭以及坏死,最终导致死亡。败血症发生的一个重要特征是肠道炎症反应和肠道上皮细胞通透性增加,从而导致革兰氏阴性菌进入宿主的循环系统。肠道炎症反应会激活一系列肠道免疫反应,例如G-蛋白偶联受体的活化。研究发现,肠道炎症反应活化多种G蛋白偶联受体,并且参与降低肠道炎症反应以及免疫应激,例如,GPR30、GPR43、GPR109A等。GPR109A是介导烟酸、丁酸、羟基丁酸等物质生物学效应的重要受体,近年来发现其与配体结合后,具有抗动脉粥样硬化、降血脂、抗炎、抗肿瘤等生物功能,被视为很多疾病治疗的新靶点。前期研究发现GPR109A作为丁酸钠的重要受体,能够保护小鼠抵抗TNBS诱导的肠道炎症反应。而在GPR109A敲除的小鼠中,丁酸钠无法发挥其保护作用。丁酸钠作为肠道微生物的重要代谢产物,对维持宿主肠道上皮细胞的紧密连接和通透性起到重要作用,此外,维持适当浓度的丁酸钠对维持肠道微生态的稳定性和多样性也不容忽视。作为维持肠道健康,降低肠道炎症反应的重要受体,GPR109A是否与肠道微生物的多样性、稳定性和代谢产物变化存在联系仍然未知。
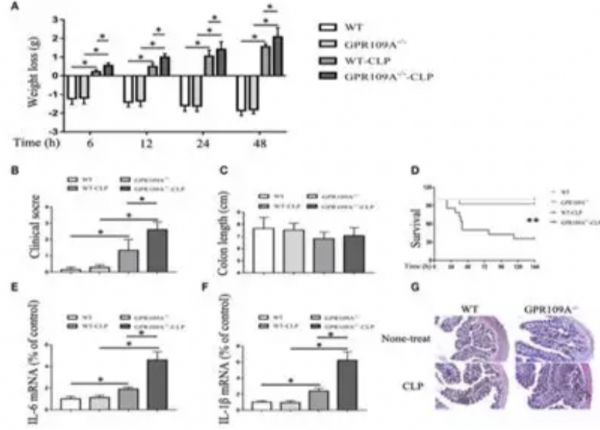
在本项研究中,来自吉林大学动物医学学院的科研人员利用WT和GPR109A敲除的小鼠,结合盲肠结扎穿刺技术建立败血症动物模型,研究发现敲除鼠与野生鼠相比,具有更严重的炎症程度和更高的致死率,且敲除鼠的肠道机械屏障与化学屏障功能都被削弱了。那么,GPR109A敲除是否对肠道微生物也产生了影响,进而对降低宿主抵抗肠道炎症反应的能力呢?吉林大学的研究人员通过和广东省微生物研究所(华南应用微生物国家重点实验室)的科研人员合作,利用16S rDNA测序技术和生物信息学分析,结果发现,野生鼠与敲除鼠在肠道菌群组成及其代谢信号通路存在显著差异,其中野生鼠拟杆菌门和放线菌门含量高于敲除鼠,而敲除鼠厚壁菌门、变形菌门(多数致病菌属变形菌门)和疣微菌门含量高于野生鼠。为进一步证实肠道菌在败血症模型中的作用,研究者通过抗生素处理和粪菌移植重建肠道微环境,进一步证实肠道微生物参与了败血症发生过程中发挥了对肠道屏障的保护作用。此研究是世界首例首次利用小鼠模型建立了GPR109A受体与肠道菌群之间的直接联系,并且,为肠道菌群分菌移植治疗肠道炎症反应提供了理论和实践依据。
作者及课题组简介
该文章的第一完成单位吉林大学动物医学学院柳巨雄教授、王玮副教授多年来一直从事G蛋白偶联受体相关研究,先后证实了GPR109A介导的神经保护、抑制肠道炎症和调控肠道机械屏障的作用。本研究合作单位广东微生物研究所(华南应用微生物国家重点实验室)谢黎炜研究员及其课题组,通过深度分析和挖掘细菌16S rDNA测序数据,进一步证实了宿主的基因型对肠道菌群的影响,为宿主-肠道菌互作理论提供了坚实的证据,也为败血症等疾病的治疗和预防提供了有益的思路。
图1 GPR109A敲除增加败血症小鼠模型死亡率
图2 GPR109A敲除诱导肠道菌群紊乱
图3 粪菌移植重建肠道微环境
原始出处:
Guangxin Chen, et al. G Protein-Coupled Receptor 109A and Host Microbiota Modulate Intestinal Epithelial Integrity During Sepsis. Frontiers in Immunology. Sep 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肠道菌#
68
#烟酸#
77
#互作#
76
学习了谢谢
97
学习了
96