OCC 2015 :李毅刚——新型口服抗凝药在房颤中的应用
2015-09-10 MedSci MedSci原创
中华医学会第十七次全国心血管大会暨第九届东方心脏病学会议(OCC2015)今天在上海世博中心隆重举行。今天上午举行的继续教育论坛心律失常场上,来自上海交通大学医学院附属新华医院心血管内科主任李毅刚发表题为《新型口服抗凝药在房颤中的应用》主题演讲,精彩内容如下: 房颤的患病率与卒中风险 房颤是最常见的心律失常,与其相关的住院事件占所有心律失常性疾病导致的住院事件的三分之一。据估计,全球罹患房颤的
中华医学会第十七次全国心血管大会暨第九届东方心脏病学会议(OCC2015)今天在上海世博中心隆重举行。今天上午举行的继续教育论坛心律失常专场上,来自上海交通大学医学院附属新华医院心血管内科主任李毅刚发表题为《新型口服抗凝药在房颤中的应用》主题演讲,精彩内容如下:
房颤的患病率与卒中风险
房颤是最常见的心律失常,与其相关的住院事件占所有心律失常性疾病导致的住院事件的三分之一。据估计,全球罹患房颤的患者人数:欧洲为600万、美国510万、中国800万;40岁及以上人群中,有将近四分之一的人会发生房颤(男性26%,女性23%)。
卒中是房颤的主要并发症,15%~20%卒中是由房颤导致。房颤患者卒中总体风险增5倍,房颤患者每年卒中发生率为3%~4%,1年内死亡率高达50%,心源性卒中30天内死亡率可达25%。无论是阵发性还是持续性房颤,患者发生卒中的风险都是一样的。
房颤相关卒中的预防
2/3由房颤引发的卒中可能通过适当的抗凝治疗进行预防,对于具有一个以上中度危险因子的患者建议使用VKA抗凝治疗(INR 2.0-3.0)。
一项汇总29项试验,28,044名患者的荟萃分析显示调整剂量的华法林能减少缺血性卒中、降低全因死亡率。房颤卒中预防中华法林优于阿司匹林。
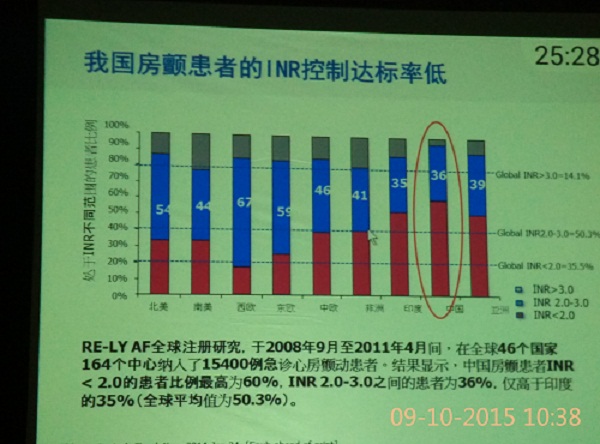
图:我国房颤患者INR控制达标率
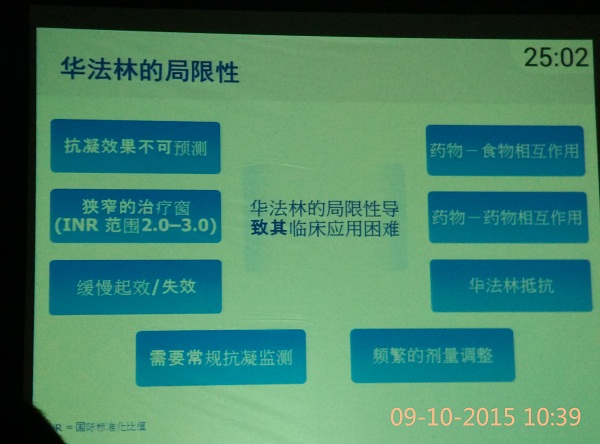
图:华法林的局限性
理想的抗凝剂
口服给药,具有可逆性
可预测的药代动力学和药效学
发生食物和药物相互作用的可能性小
固定剂量给药,在低剂量阈值时即有效,只在高剂量阈值时才出现出血并发症
治疗窗宽
无需定期监测
合理的费用有
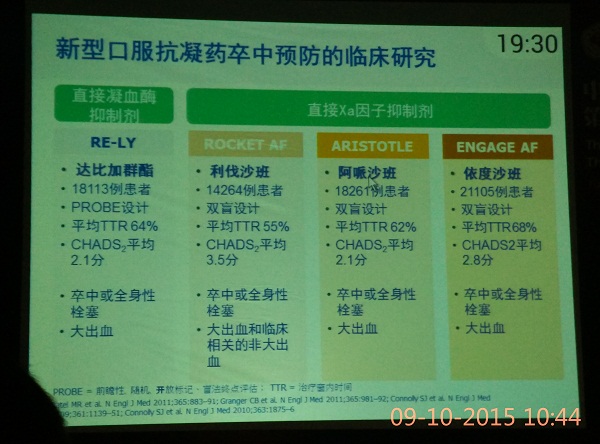
图:新型口服抗凝药卒中预防的临床研究
指南中推荐
2012年ESC房颤治疗指南中关于非瓣膜病房颤抗凝策略中应用CHA2DS2-VASc评分评估卒中风险,评分=1的患者,基于对其出血风险的评估和自身的选择,考虑给予口服抗凝治疗。2014 AHA/ACC/HRS指南也采用了这一评分方法,评分=1的非瓣膜性房颤可以考虑不抗栓、口服抗凝药或阿司匹林治疗,评分>=2且慢性肾脏病达终末期或接受透析治疗,可以使用华法林抗凝治疗。且在此指南中将三种NOAC(达比加群、利伐沙班、阿呱沙班)均纳入推荐。
总结:
1.房颤显著增加卒中发生风险,增加患者的致残、致死率
2.由于华法林的局限性导致我国抗凝治疗不足、治疗依从性差,因此迫切需要新的口服抗凝药物
3.多项循证证据证实,新型口服抗凝药物在预防卒中方面非劣效或估于华法林,不增加甚至降低出血的风险
4.国内外权威房颤治疗指南推荐的房颤患者抗凝治疗中,新型口服抗凝药物有望逐渐取代华法林
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新型口服抗凝药#
91
#OCC#
74
#口服抗凝药#
77
这样的文章很有意义
147