Cardiovasc Diabetol:2型糖尿病患者需要住院治疗的营养生物标志物与心力衰竭
2022-06-21 从医路漫漫 MedSci原创
糖尿病患者患冠状动脉疾病(CAD)和糖尿病心肌病的风险过高,这是导致心力衰竭(HF)的两个主要原因。
背景:糖尿病是一种全球性的疾病,预计到2030年全球将有超过10%的人受到影响。除了微血管并发症,心血管疾病是糖尿病患者发病率和死亡率的主要原因之一。糖尿病患者患冠状动脉疾病(CAD)和糖尿病心肌病的风险过高,这是导致心力衰竭(HF)的两个主要原因。最近,一项对超过1200万人进行的大型荟萃分析证实,无论男女,2型糖尿病(T2D)患者发生心衰的风险是非2型糖尿病患者的两倍。在与这种复杂疾病相关的多种因素中,营养似乎是必不可少的,因为它是预防和/或治疗行动的可能目标,是T2D和HF的可改变的危险因素。在这方面,血糖指数和负荷最近在一项大规模的全球流行病学方法中被证明与心血管疾病有关。然而,当仔细研究不同结果的影响时,结果发现血糖指数和负荷与动脉粥样硬化相关的心血管事件有关,但与心衰无关。
到目前为止,营养在HF中的影响往往被低估。在ESC(欧洲心脏病学会)的指南中,HF的营养主要与营养不良和肥胖有关,而肥胖是HF的贡献者。饮食建议主要集中在盐的摄入、健康饮食、保持体重以及在中毒性心肌病的情况下避免过量饮酒。我们先前证明了红肉消费的标记物(三甲胺N-氧化物[TMAO]和相关代谢物)与T2D患者的主要不良心血管事件(MACE)的发生以及死亡率之间的关联。然而,我们没有评估营养生物标记物对心力衰竭的影响,心力衰竭是糖尿病患者的关键结局。
2019年的一项倡议--Eat-Lancet健康饮食委员会建议考虑普遍健康饮食的14个关键项目[8]。能够识别与心力衰竭相关的营养生物标志物是一个重要的问题,尤其是在T2D中。这尤其能够及早查明易患心力衰竭的患者,并可考虑对其采取预防性的具体管理措施,包括营养咨询。这种方法可以为T2D患者的个性化营养铺平道路。
目的:评估基线营养生物标志物与红肉摄入量(TMAO及其相关化合物,即三甲胺、甜菜碱、胆碱和肉碱)和蔬菜摄入量(硫代氨基酸:半胱氨酸、同型半胱氨酸和蛋氨酸)如何与T2D患者需要住院的心力衰竭(HFrH)发生率相关,而与他们的心力衰竭病史无关。
方法:我们采用了SURDIAGENE(生存糖尿病和遗传学)研究,这是一项大型、前瞻性、单中心队列研究,包括2001至2012年间的1468名T2D患者。TMAO及其前体(三甲胺、甜菜碱、胆碱和肉碱)以及硫代氨基酸(半胱氨酸、同型半胱氨酸和蛋氨酸)的测定采用液-质联用法。主要结果是需要住院的心力衰竭(HFrH),定义为导致住院和/或死亡的第一例急性心力衰竭,由一个裁决委员会根据2015年12月31日之前的医院记录确定。次要结局为复合事件HFrH和/或心血管死亡和全因死亡。生物标记物和预后之间的关联使用特定原因的危险模型进行研究,该模型调整了年龄、性别、冠状动脉疾病病史、NT-proBNP、CKD-EPI来源的EGFR和尿白蛋白/肌酐比率。危险比(HR)表示为一个标准差。
结果:1349/1468名SURDIAGENE参与者(91.9%)获得了感兴趣的数据,其中包括569名女性(42.2%),平均年龄为64.3±10.7岁,中位随访时间为7.3年[第25-75百分位数,4.7-10.8]。HFrH 209例(15.5%),HFrH和/或心血管死亡341例(25.3%),全因死亡447例(33.1%)。在未调整的危险模型中,肉碱(HR=1.20,95%CI[1.05;1.37])、甜菜碱(HR=1.34,[1.20;1.50])、胆碱(HR=1.35,[1.20;1.52])、TMAO(HR=1.32,[1.16;1.50])、半胱氨酸(HR=1.38,[1.21;1.58])和同型半胱氨酸(HR=1.28,[1.17;1.39])与HFrH有关,但与TMA和蛋氨酸无关。在完全调整的模型中,当同型半胱氨酸仅与全因死亡正相关(HR=1.16,[1.06;1.27])时,这些关联都不显著,对HFrH和HFrH和/或心血管死亡也不显著。
表1感兴趣的营养生物标志物的基准值,按后续事件的状况分类

表2 HFrH、HFrH和/或CV复合死亡事件及全死因死亡的生存分析
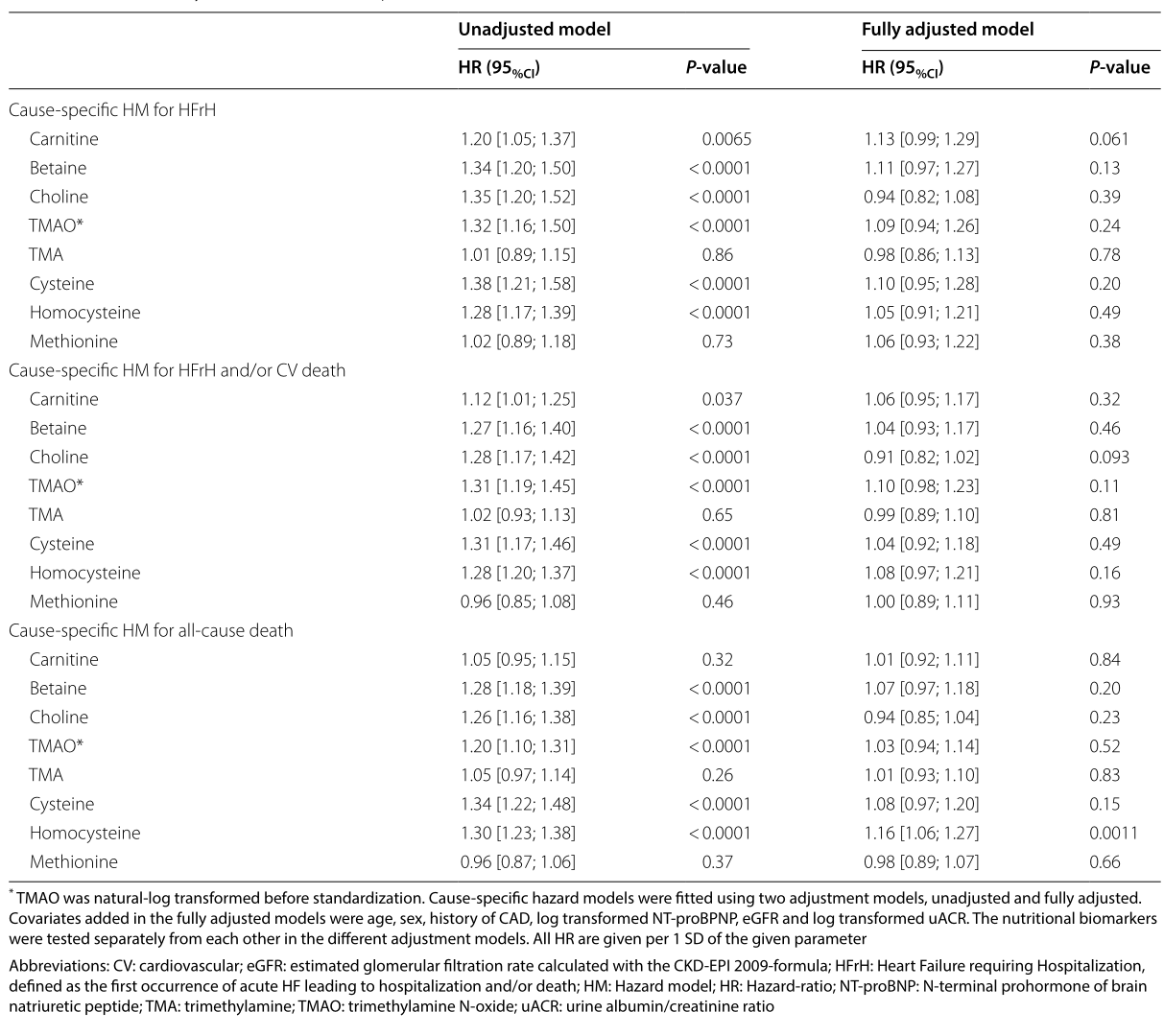
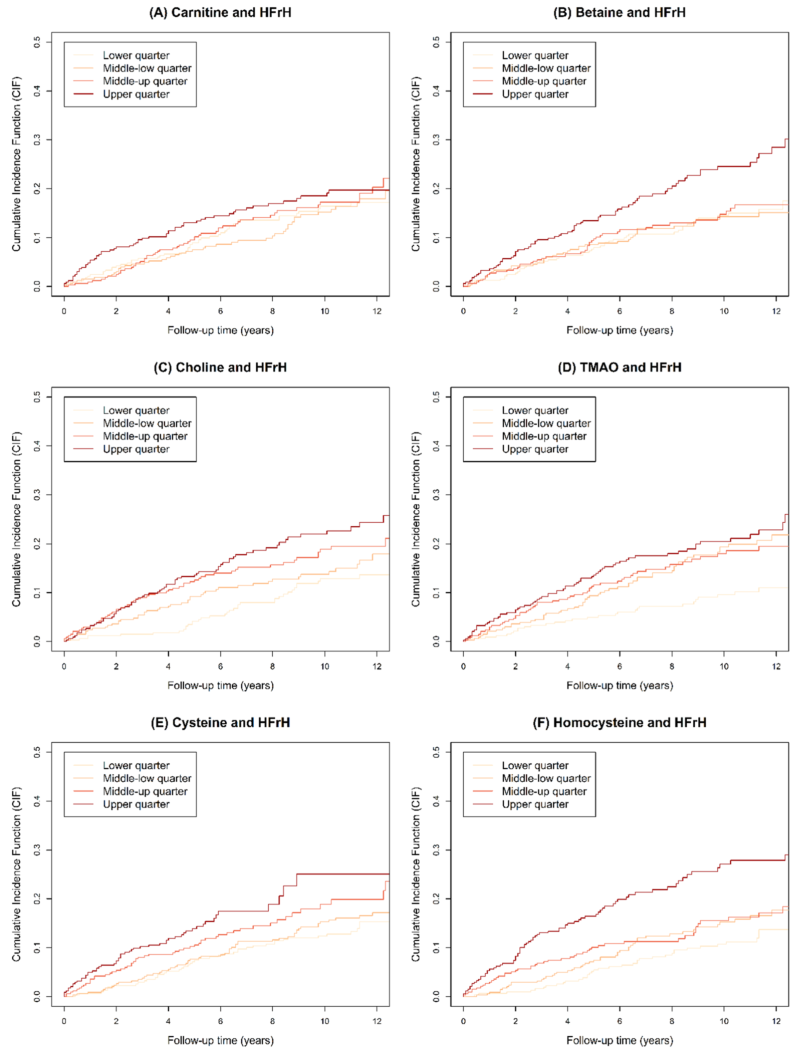
图1 HFrH的累积关联函数。不同感兴趣参数的四分位数:肉碱(中位数=42.6,[25-75]百分位数=[35.4-50.7]);甜菜碱(31.5,[24.6-38.9]);胆碱(1.43,[1.22-1.68]);TMAO(6.8,[4.2-12.8]);半胱氨酸(23,[13-39]);同型半胱氨酸(8.9,[4.7-14.8])。HFrH:需要住院治疗的心力衰竭,定义为首次发生导致住院和/或死亡的急性心衰;TMAO:三甲胺N-氧化物
结论:除常见的心脏和肾脏相关危险因素外,TMAO及其前体似乎不是HFrH的重要预后因素,而同型半胱氨酸是T2D患者全因死亡的独立危险因素。
原文出处:Wargny M, Croyal M, Ragot S, et al.Nutritional biomarkers and heart failure requiring hospitalization in patients with type 2 diabetes: the SURDIAGENE cohort.Cardiovasc Diabetol 2022 Jun 09;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
78
#BET#
78
#标志物#
82
#ASC#
81
#2型糖尿病患者#
89
#糖尿病患者#
75
#生物标志#
84
#生物标志#
83