JACC:新型抗凝药利伐沙班减少外周动脉血管重建后的首次及总缺血事件
2021-07-24 MedSci原创 MedSci原创
综上,接受LER治疗的有症状的PAD患者有很高的总事件负担,使用利伐沙班可以显著减少。
周围动脉疾病(PAD)患者发生主要不良肢体和心血管事件的风险较高。下肢血运重建(LER)与肢体不良事件的风险明显升高有关,甚至在手术后几年也是如此。最近,有人描述了血管重建后急性PAD患者的风险状况,显示干预后早期肢体不良的风险明显升高。
VOYAGER PAD(利伐沙班在降低有症状的外周动脉疾病患者接受下肢血管重建手术的主要血栓性血管事件风险方面的有效性和安全性)研究表明,尽管所有患者都接受了阿司匹林治疗,80%的患者接受了他汀类药物治疗,1/2的患者接受了氯吡格雷治疗,但在3年后,大约20%的接受LER的患者出现了第一次不良肢体或心血管事件。

然而,在阿司匹林治疗基础上加用利伐沙班2.5mg,每天两次,与单独使用阿司匹林相比,首次事件减少了约15%,在3年内预防首次事件所需的治疗数量为39。然而,这些研究结果并没有报告后续事件的发生率以及利伐沙班对减少总事件的影响。
因此,该人群中的总事件(即首次和可能的后续事件)发生率以及利伐沙班对总事件的益处尚不清楚。为此,来自德国法兰克福心血管中心的专家开展了相关研究,结果发表在JACC杂志上。
本研究旨在评估LER后PAD患者血管事件的总负担以及低剂量利伐沙班对总事件的疗效。VOYAGER PAD将接受LER治疗的PAD患者随机分配到利伐沙班2.5毫克,每天两次加阿司匹林或单独使用阿司匹林。
主要终点是首次发生急性肢体缺血、血管性重大截肢、心肌梗死、缺血性中风或心血管死亡事件的时间。目前的分析考虑了主要终点组成部分的所有事件(首次和后续),以及额外的血管事件,包括外周血管再通和静脉血栓栓塞。
按第一次非致命性血管事件的类型划分的第二次血管事件的发生率
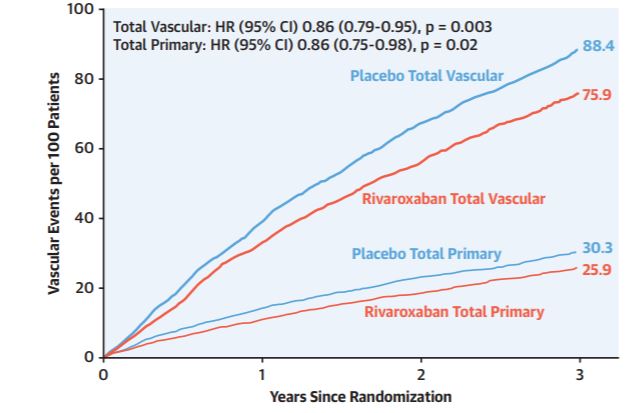
在6564例随机事件中,共有4714例首次和后续血管事件,包括1614例主要终点事件和3100例其他血管事件。利伐沙班分别减少了14%主要终点事件(HR=0.86;95%CI:0.75-0.98)和14%血管事件总数(HR=0.86;95%CI:0.79-0.95)。
使用利伐沙班在3年内估计每100名参与者可避免4.4次初级和12.5次血管事件。由此可见,总事件的减少可能是量化利伐沙班在这种情况下的疗效的一个有用指标。
原发事件总数和血管事件总数的累积数量
综上,接受LER治疗的有症状的PAD患者有很高的总事件负担,使用利伐沙班可以显著减少。
参考文献:
Total Ischemic Event Reduction With Rivaroxaban After Peripheral Arterial Revascularization in the VOYAGER PAD Trial. J Am Coll Cardiol. 2021 Jul, 78 (4) 317–326
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
112
#学习#收益良多
90
#新型抗凝药#
112
#动脉血#
92
非常好,已收藏
143
#ACC#
0
#外周动脉#
91
非常受用
82