ESMO Open:抗PD-(L)1抗体治疗转移性尿路上皮癌的预后
2021-03-20 MedSci原创 MedSci原创
质子泵抑制剂的使用与抗PD-(L)1治疗的转移性尿路上皮癌患者的预后较差相关?!
在日常临床实践中,很少有研究探讨抗PD-(L)1抗体在转移性尿路上皮癌(mUC)中的安全性和有效性。目前,关于基线临床和分析因素对治疗结果的影响的了解很少。
这是一项多中心的回顾性研究,招募了119名既往接受过和没接受过抗PD-(L)1治疗的mUC患者,旨在探究抗PD-(L)1单一治疗的安全性和有效性,并确定影响治疗预后的预处理因素。此外,还开发了一个独立的总生存期(OS)预后模型,并在内部进行了验证。
总人群的治疗疗效
中位OS为7.8个月(95%CI 5.4~10.4),中位无进展生存期(PFS)为2.80个月(95%CI 2.4~3.4),疾病控制率(DCR)为40%(95%CI 31~49),总有效率(ORR)为24%(95%CI 15~31)。
腹膜转移与OS不良相关(危险比[HR] 2.40,95%CI 1.08~5.33;P=0.03]。质子泵抑制剂的使用与较差的OS(HR 1.83,95%CI 1.11~3.0 2;P=0.02)和PFS(HR 1.94,95%CI 1.2~3.09;P=0.005)、较低的DCR(OR 0.38,95%CI 0.17~0.89;P=0.03)和ORR(OR 0.18,95%CI 0.02~1.6 0;P=0.002)相关。
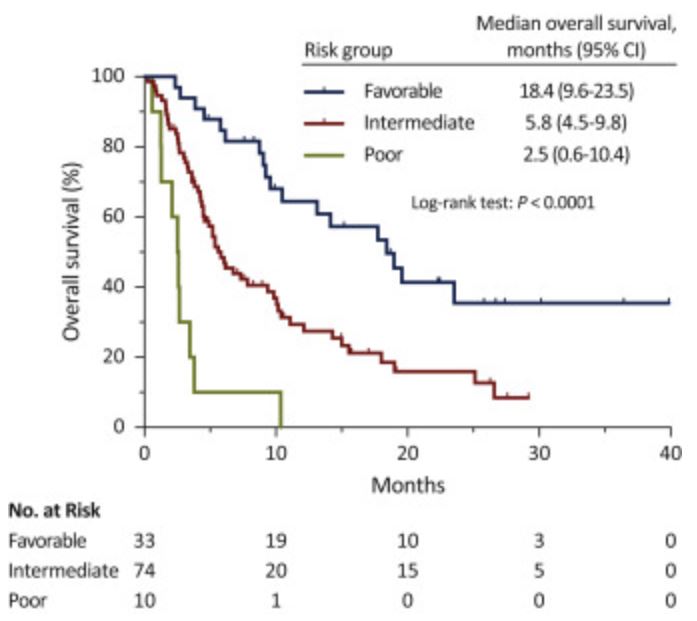
不同风险组患者的预后
建立的3个风险类别预后模型纳入了ECOG表现状态、PPI使用情况、白蛋白水平、有无肝转移和腹膜转移,与较高的死亡风险相关(HR 3.0,95%CI 1.97~4.56;P=0.0001)。
综上,本研究证实,在mUC患者的日常临床治疗中,抗PD-(L)1单一疗法是一种安全有效的治疗选择。本研究提示腹膜转移是这类患者的OS的一个独立的预后因素,并强调了PPI的使用与较差的治疗预后相关。
原始出处:
Ruiz-Baobre J,Molina-Díaz A,Fernández-Calvo O et al. Rethinking prognostic factors in locally advanced or metastatic urothelial carcinoma in the immune checkpoint blockade era: a multicenter retrospective study. ESMO Open, 2021, 6: 100090.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#PE#
57
#SMO#
50
需要看哪些指标?
92
#ESMO#
69
#转移性#
59
#转移性尿路上皮癌#
66
#上皮癌#
47
不错
83