JOT:下肢骨折患者静脉血栓栓塞症的预防
2015-05-25 MedSci MedSci原创
背景:先前研究发现,对单一膝下骨折的病人行静脉造影检查,在被检查患者中有10%–40%可以发现其罹患无症状深静脉血栓。然而,因为条件上的限制,无法对每个此类患者常规进行静脉造影检查,所以深静脉血栓症在临床上的发病率仍属未知,其对患者的风险程度亦无法把握。在不同指南中提到的常规血栓预防措施对患者的正面作用及相关的临床实践指导都有所不同。方法:在本次多中心、双盲实验中,265位有手术指证的单一膝下骨折
背景:先前研究发现,对单一膝下骨折的病人行静脉造影检查,在被检查患者中有10%–40%可以发现其罹患无症状深静脉血栓。然而,因为条件上的限制,无法对每个此类患者常规进行静脉造影检查,所以深静脉血栓症在临床上的发病率仍属未知,其对患者的风险程度亦无法把握。在不同指南中提到的常规血栓预防措施对患者的正面作用及相关的临床实践指导都有所不同。
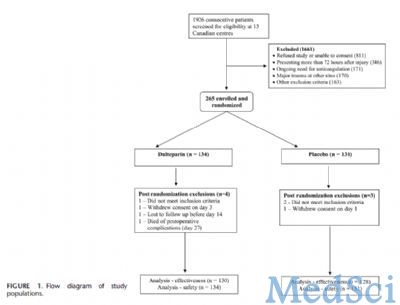
方法:在本次多中心、双盲实验中,265位有手术指证的单一膝下骨折患者被随机分到试验组和安慰剂组,试验组每日皮下注射低分子肝素5000单位。行抗血栓治疗两周后行双下肢远端静脉多普勒超声检查,并在6周和3个月时候分别进行随访,随访内容包括患者是否仍有相关症状及是否再次就诊。
本次试验在评价疗效方面的相关主要结局是“有临床意义的静脉血栓栓塞” (clinically important venous thromboembolism / CIVTE),定义为术后3个月内有症状的静脉血栓栓塞和多普勒超声发现的深静脉栓塞。关于治疗安全性的主要结局是患者是否并发大出血,时限为从预防开始时的首剂直到末剂结束后2天,大出血的定义是对患者生命产生危害的或需要外科处理的关键脏器或主要关节致命的明显出血;出血后48小时内患者需要输血1个或多个单位或血红蛋白减少20 g/L以上。
结果:最后共有258位患者(97%)的治疗情况纳入分析 (低分子肝素组130例;安慰剂组128例)。低分子肝素组和安慰剂组的CIVTE的发病率分别是1.5%和2.3%(试验组较对照组绝对风险减少0.8%,可信区间:22.0-3.0)。致死性的肺栓塞或大出血均未出现。

结论:总的术后CIVTE发病率,包括单独的胫骨、腓骨和踝关节骨折患者,较其他研究均偏低(1.9%; 95%可信区间:0.7–4.7)。在低分子肝素组和安慰剂组的患者之间,无论是CIVTE的发病率或者是治疗的安全性均未发现明显的的差异。患者招募在第一次期中分析时即停止。本次试验还提示了在研究静脉血栓栓塞症时采用不同的研究方法,基于患者的静脉造影结果或临床表现情况,会使实验结果产生显著差异。
原始出处:
Selby R1, Geerts WH, Kreder HJ, Crowther MA, Kaus L, Sealey F.A double-blind, randomized controlled trial of the prevention of clinically important venous thromboembolism after isolated lower leg fractures.J Orthop Trauma. 2015 May;29(5):224-30. doi: 10.1097/BOT.0000000000000250.
本文系Medsci原创编译整理!转载需要先获得授权,并附原文链接。谢谢!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错,赞一个
131
实用
205
临床很多血栓患者
142
关键在于预防
112
很值得学习
175
不错,学习了
99
#静脉血#
62
不错的
89
#栓塞症#
86
#静脉#
62