Mov Disord.:7T磁共振发现REM期睡眠行为障碍患者脑干核间结构连接受损
2022-01-07 影像小生 MedSci原创
该研究的发现的人类iRBD的脑干核连接受损图扩展了动物模型,是研究和评估前驱共核病分期的一个有前途的工具。
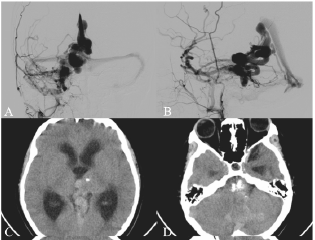
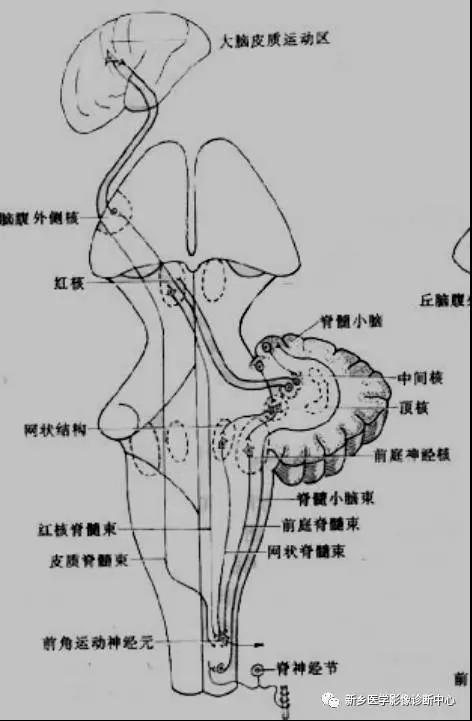
快速眼动(REM)睡眠行为障碍(iRBD)是α共核蛋白病的早期表现之一。在动物模型中已经描述了REM睡眠行为障碍的脑干病理生理学基础,但由于缺乏在体脑干核图谱和有限的磁共振成像(MRI)敏感性,在人身上的研究还不够。
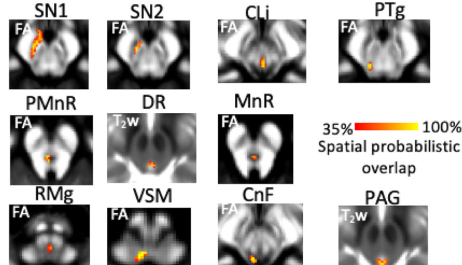
María G. García-Gomar等利用活体概率脑干核团图谱和7TMRI研究iRBD患者脑干结构连接的变化。

该研究对12例iRBD患者和12例对照患者的结构连接进行概率示示。采用双侧Wilcoxon秩和检验比较各组间的结构连接指标。
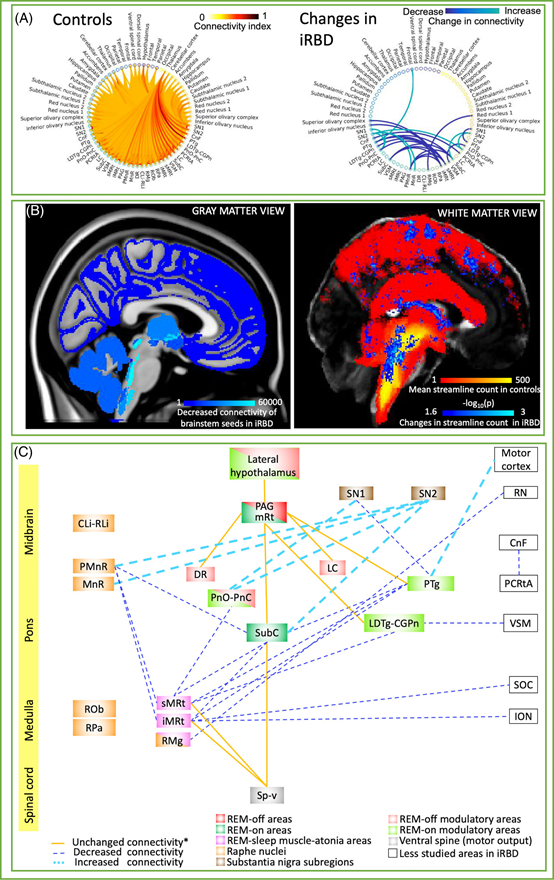
iRBD中脑干14个核核的结构连接受损(Z = 2.6, P<0.01),包括REM-on区和REM睡眠肌张力减退区之间的连接。
目前对iRBD生理病理知识的理解主要来自动物研究,因为有几个因素阻碍了对人活体这种睡眠障碍的研究,主要是缺乏一个图集来精确定位活体的小脑干结构,以及扩散MRI的灵敏度/分辨率有限。该研究结果克服了这两个限制,通过将原始脑干核图映射到活体的高空间分辨率HARDI(7T)。
该研究的发现的人类iRBD的脑干核连接受损图扩展了动物模型,是研究和评估前驱共核病分期的一个有前途的工具。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#REM#
69
#Disord#
63
#行为障碍#
65
#Dis#
42
#磁共振#
43