患者男性,62岁,因出现顽固性肠梗阻及腹痛一周余而到急诊科就诊。
据该患者称,他既往有过6年的持续性腹膜透析和10年的血液透析病史。
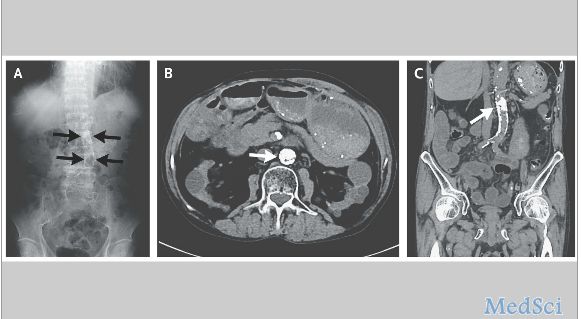
腹部X线检查(图A)和计算机断层扫描(图B和图C显示轴位、冠状位)显示明显的腹主动脉壁钙化(箭头处)接近完全闭塞,另外肠系膜上动脉重度狭窄。
超声心动图显示主动脉瓣严重狭窄并伴有中度返流,二尖瓣狭窄与关闭不全及三尖瓣返流。
会诊医师认为,该患者主动脉严重狭窄、肠系膜上动脉狭窄是肠梗阻形成的诱发因素,但是,肠系膜上动脉旁路腹主动脉全置换也可能是发病的风险因素之一。
最后,该患者进行了主动脉瓣置换术及二尖瓣、三尖瓣成形术。术后不久,该患者腹部的肠梗阻症状逐渐消退。
原始出处:
Yoko Ito, M.D., Ph.D., and Akihiko Nogami, M.D., Ph.D. Aortic Calcification and Superior-Mesenteric-Artery Stenosis N Engl J Med 2016; 375:566August 11, 2016
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉钙化#
35
值得学习
51
继续学习
0
继续关注
73
继续学习
52
继续学习
61
#主动脉#
29
#动脉狭窄#
42
#肠系膜#
38