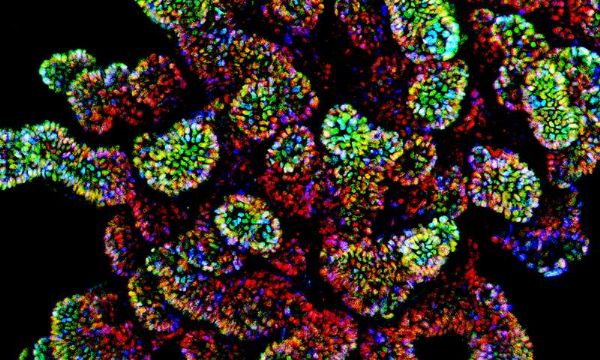
Nat Med:科学家研发出更好检测结肠癌药物的人体组织模型!
2017-06-21 枫丹白露 来宝网
Weill Cornell Medicine研究人员开发了首例“培养皿”中针对源自干细胞的人类结肠癌模型的“疾病”平台,允许他们识别常见的遗传形式的疾病的靶向药物治疗。该发现还克服了使用小鼠研究这种癌症的长期挑战,因为它们通常不会发展该疾病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
74
#研发#
64
#Med#
87
不错的方式,努力学习,刻苦专研,不断总结出来新经验。给点个赞!
91
谢谢分享。
99
希望早点投用到患者手中
79