EHJ:中年妇女猝死主要原因——自发性冠状动脉夹层患者的抗血小板疗法单抗更佳!
2021-08-02 MedSci原创 MedSci原创
在1年的随访中,与SAPT相比,DAPT与较高的心血管不良事件率独立相关。
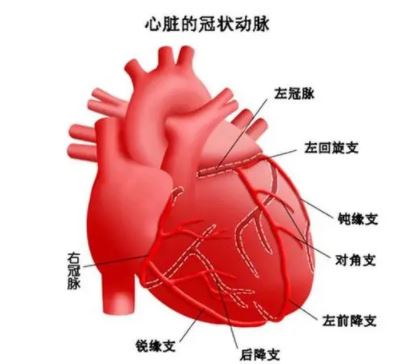
自发性冠状动脉夹层(SCAD)是一种既非创伤性亦非医源性的冠状动脉管壁分离,为急性心肌梗死(AMI)的罕见病因。该病在较年轻的患者和女性患者中更常见,是40~65岁女性急性冠状动脉综合征(ACS)和猝死的主要原因。
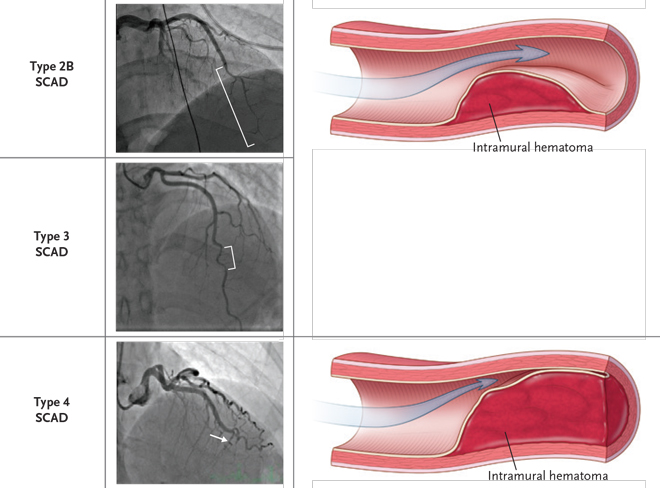
NA-SCAD的潜在发病机制尚未完全明确,但目前提出了两种机制,即冠状动脉内膜撕裂或冠状动脉滋养血管出血伴中膜内出血。动脉粥样硬化型冠状动脉夹层是一种机制不同的SCAD变异型,并且通常会因中膜萎缩和瘢痕形成限制其病变范围。
研究证实,21%~27%的妊娠心肌梗死和50%的产后冠状动脉事件与SCAD相关。此外,SCAD是引起ACS的原因之一。流行病学调查发现,在所有血管造影结果中SCAD诊断率为0.07%~0.2%,且ACS患者的冠状动脉造影中占2%~4%。
目前有关标准ACS药物治疗对SCAD患者的疗效仍然存在争议。其中主要集中在抗凝以及抗血小板药物的治疗:虽有病例报道了SCAD溶栓治疗成功的个别先例,但也有报道指出溶栓会加剧壁内血肿甚至冠状动脉破裂导致溶栓治疗后心脏压塞。
鉴于在接受初始保守治疗的SCAD患者中,抗血小板治疗的作用仍是一个争论的问题,来自意大利图灵大学的专家开展了相关研究,旨在评估SCAD患者的抗血小板药物使用情况,并研究单一(SAPT)和双重(DAPT)抗血小板方案与1年患者预后之间的关系。结果发表在《欧洲心脏病杂志》EHJ上。
研究人员调查了纳入DISCO多中心国际注册的SCAD患者的1年疗效。根据SAPT或DAPT处方,将患者分为两组。主要终点是12个月的主要不良心血管事件(MACE)发生率,定义为全因死亡、非致命性心肌梗死(MI)和任何非计划性经皮冠状动脉介入(PCI)的综合。
在DISCO登记的314名患者中,共纳入了199名接受保守治疗的SCAD患者。大多数患者为女性(89%),表现为ACS(92%),平均年龄为52.3±9.3岁。67人(33.7%)接受了SAPT治疗,132人(66.3%)接受了DAPT治疗。62.9%的DAPT患者使用阿司匹林加氯吡格雷或替卡格雷,36.4%的DAPT患者使用氯吡格雷。
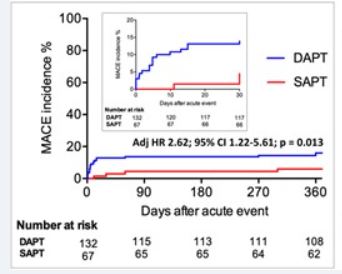
随访期间,SAPT与DAPT两组MACE累积发生率
总体而言,在12个月的随访中,观察到14.6%的MACE率。接受DAPT治疗的患者的MACE率比接受SAPT治疗的患者高162%(18.9% vs. 6.0%,HR=2.62;95% CI:1.22-5.61)。经分析这主要是由于早期非致命性MI或非计划性PCI过多。
在多元回归分析中,2a型SCAD(OR=3.69;95% CI 1.41-9.61)和DAPT方案(OR=4.54;95% CI 1.31-14.28)导致与12个月MACE的高风险独立相关。
SAPT与DAPT两组发生主要心血管事件情况
由此可见,大多数接受初始保守治疗的SCAD患者接受DAPT。然而,在1年的随访中,与SAPT相比,DAPT与较高的心血管不良事件率独立相关。
参考文献:
Antiplatelet therapy in patients with conservatively managed spontaneous coronary artery dissection from the multicentre DISCO registry, European Heart Journal, 2021;, ehab372, https://doi.org/10.1093/eurheartj/ehab372
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠状动脉夹层#
90
#动脉夹层#
115
#自发性#
88
获益匪浅
107
受益匪浅,多谢分享
104
学习了,谢谢分享
154