Nature:根据SLAMF7蛋白的表达决定是否使用anti-CD47治疗淋巴癌
2017-04-26 MedSci MedSci原创
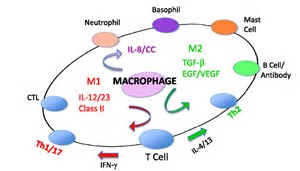
多种的CD47蛋白在多种B细胞肿瘤细胞中都有较高的表达,而SLAMF7蛋白的表达量则不是很一致。鉴于多项阻断CD47结合SIRP-a的临床研究正在进行,因此通过检测肿瘤组织中的SLAMF7蛋白的表达量能为是否使用阻断CD47-SIRP-a疗法提供参考,从而制定更加个性化的治疗方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#LAM#
32
#CD4#
40
#Nat#
70
学习了,感谢分享!
46
#淋巴癌#
38
#SLAMF7#
44