癌症很快会成为21世纪每个国家的主要死亡原因。本研究旨在分析1990-2019年204个国家或地区29种癌症的发病率和死亡率,以指导全球的癌症预防和控制策略。
研究人员从2019年的全球疾病负担研究中收集了29种癌症团体的详细信息。按性别、年龄、地区和国家分层计算29种癌症的年龄标准化发病率 (ASIR) 和年龄标准化死亡率 (ASDR)。此外,对常见癌症类型进行单独分析。
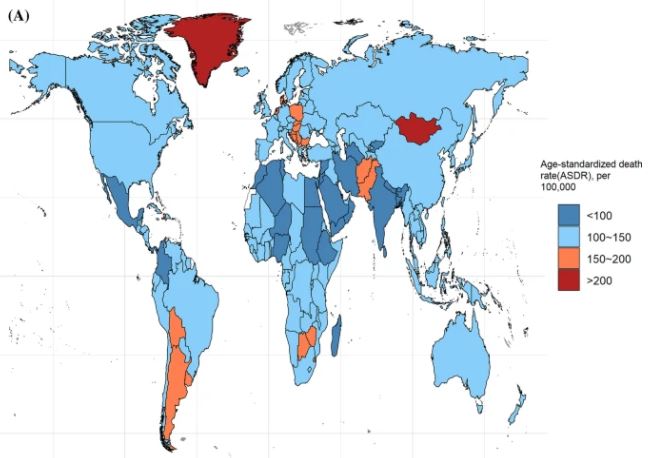
2019年全球癌症的总年龄标准化死亡率
2019年,全球约有1000多万人死于癌症,大约是1990年的两倍。气管、支气管和肺癌 (TBL) 的总体死亡率最高,胰腺癌的年龄标准化死亡率升高了24%,是病死率最高的癌症 (CFR)。全球癌症的年龄标准化发病率呈上升趋势,睾丸癌、甲状腺癌、恶性皮肤黑素瘤呈显著上升趋势。男性癌症的年龄标准化发病率和年龄标准化死亡率约为女性的1.5倍。
2019年全球癌症的致死率
50岁以上的人群患癌症的风险最高,该年龄组的发病率和死亡率占所有年龄组癌症发病率和死亡率的85%以上。由于人口密度高,亚洲是癌症负担最重的地区,该地区食管癌死亡人数占全世界食管癌死亡人数的53%。
此外,根据世界银行人类发展指数 (HDI),大多数癌症的死亡率和发病率随着社会人口指数的增加而升高。最后,全球不同国家的癌症特征各不相同。
全球癌症相关死亡病例数的变化趋势
总之,全球癌症负担持续增加,不同区域、年龄、国家、性别和癌症类型之间的死亡率和发病率存在很大差异。有效的、因地制宜的癌症预防和控制措施对减少未来全球癌症负担至关重要。
原始出处:
Lin Longfei,Li Zhiyong,Yan Lei et al. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990-2019.[J] .J Hematol Oncol, 2021, 14: 197.https://doi.org/10.1186/s13045-021-01213-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Oncol#
67
#发生率#
88
#EMA#
74
学习
106
或病人有胸痛时,立即停药及时
98