Eur Neurol:脑室周围白质高信号可预测其边缘梗死
2015-12-21 phylis 译 MedSci原创
背景:白质高信号(WMH)预测卒中和新的腔隙性梗死的发生;此外,WMH也影响梗死部位。这篇研究旨在确定WMH和急性腔隙性脑梗死之间的空间关系。方法:共有590名幕上区急性腔隙性梗死的患者。进行轴位和冠状位MRI评估梗死和WMH的四种情况:与WMH无接触(0级),接触不重叠(Ia级),部分重叠(Ib级)和完全重叠(II级)。此外,研究者定义Ia级,Ib级梗死定义为边缘部位梗死,并且调查其预测因子极其
背景:白质高信号(WMH)预测卒中和新的腔隙性梗死的发生;此外,WMH也影响梗死部位。这篇研究旨在确定WMH和急性腔隙性脑梗死之间的空间关系。
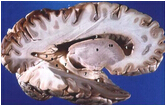
方法:共有590名幕上急性腔隙性脑梗死的患者。进行轴位和冠状位MRI评估梗死和WMH的四种情况:与WMH无接触(0级)、接触不重叠(Ia级)、部分重叠(Ib级)和完全重叠(II级)。此外,研究者定义Ia级,Ib级梗死定义为边缘部位梗死,并且调查其预测因子极其短期预后。
结果:47.9%(283)的患者为Ia级和Ib级(Ia级= 27.6%,IB级= 20.3%);51.5%(304)名为0级;只有0.5%(3)为II级。与非边缘梗死患者相比,边缘梗死患者的入院梗死面积较大,WMH较严重,NHISS分数较高,BI分数较低。边缘梗死患者出院分数也较低。皮质下白质梗死,弥散加权成像面积,脑室周围WMH及深部WMH是边缘梗死的预测因子。
结论:半数腔隙性脑梗死位于WMH边缘。脑室周围WMH和深部WMH是边缘局部梗死的预测因子。
原文出处:
Zhang X, Ding L, et al. Spatial Relationship between Acute Lacunar Infarction and White Matter Hyperintensities. Eur Neurol.2015 Dec 9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#白质#
83
#高信号#
80
#Neurol#
68
值得收藏,学习,谢谢分享
157
#白质高信号#
66
#脑室#
92