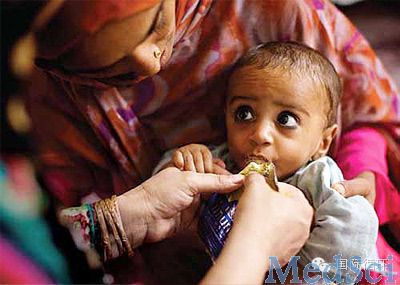
Hypertension:儿童期严重营养不良会使成年后舒张压和血管阻力增高
2014-07-02 国际循环 国际循环
最新研究显示,儿童时期严重急性营养不良者,成年后会有心脏结构和功能异常,导致舒张压水平更高,并增加外周血管阻力。 Ingrid Tennant博士(牙买加热带医学研究所)表示,“研究结果对世界上大量曾经营养不良者非常重要……这些效果可能起源于出生前,但也可能由童年时营养缺乏所致或加剧。”研究6月30日在线发表于Hypertension。 研究入选116例儿童时期严重急性营养不良,并存活至成年的
Ingrid Tennant博士(牙买加热带医学研究所)表示,“研究结果对世界上大量曾经营养不良者非常重要……这些效果可能起源于出生前,但也可能由童年时营养缺乏所致或加剧。”研究6月30日在线发表于Hypertension。
研究入选116例儿童时期严重急性营养不良,并存活至成年的受试者。分析中包括两种营养不良临床综合征,即严重蛋白质缺乏的恶性营养不良、热量与蛋白质不足的消瘦型营养不良。
与45例年龄、性别、体重指数匹配的对照者相比,童年时严重营养不良者左室流出道直径、每搏输出量、心输出量和脉搏波传导速度显著降低,舒张压水平高4.3 mm Hg,全身血管阻力显著较高。研究者表示该结果“令人惊讶”,可能与同样收缩压水平下,较低的心输出量的舒张压较高相关。
研究者总结,“然而,无论潜在机制如何,两种严重急性营养不良都与心血管风险增高相关是十分明确的。”
原始出处:
Tennant IA, Barnett AT, Thompson DS, Kips J, Boyne MS, Chung EE, Chung AP, Osmond C, Hanson MA, Gluckman PD, Segers P, Cruickshank JK, Forrester TE.Impaired Cardiovascular Structure and Function in Adult Survivors of Severe Acute Malnutrition.Hypertension. 2014 Jun 30. pii: HYPERTENSIONAHA.114.03230.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TENS#
70
#PE#
80
#舒张压#
99
#Hypertension#
80
#增高#
0
#增高#
79