Cell Host Microbe:I型干扰素b的病毒清除机制研究
2015-05-18 佚名 生物谷
I型干扰素在宿主抵抗微生物感染的先天免疫与后天免疫过程中都具有重要的作用。包括控制病原体的状态,调节先天免疫反应,激活后天免疫反应等等。尽管如此,一些研究发现I型干扰素能够提高感染的严重程度。之前的研究发现I型干扰素的阻断能够促进病毒感染后的清除,而这一效应主要是通过营造免疫抑制的环境实现的,主要包括:1、促进一些负向调控因子,如IL-10,PD-1的产生;2、破坏脾脏的结构;3,抑制淋巴细胞

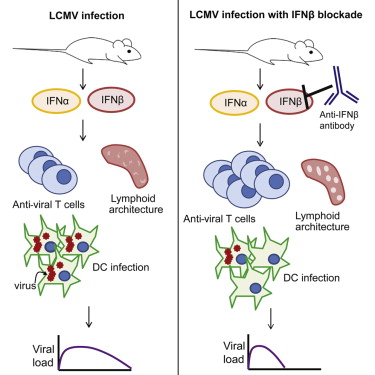
I型干扰素在宿主抵抗微生物感染的先天免疫与后天免疫过程中都具有重要的作用。包括控制病原体的状态,调节先天免疫反应,激活后天免疫反应等等。尽管如此,一些研究发现I型干扰素能够提高感染的严重程度。之前的研究发现I型干扰素的阻断能够促进病毒感染后的清除,而这一效应主要是通过营造免疫抑制的环境实现的,主要包括:1、促进一些负向调控因子,如IL-10,PD-1的产生;2、破坏脾脏的结构;3,抑制淋巴细胞向脾脏的迁移。然而,目前对于哪一类I型干扰素具有这一功能仍不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Micro#
47
#机制研究#
64
#Cell#
53
#CEL#
57
#CRO#
55
#I型干扰素#
82