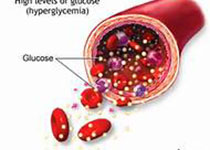
JCEM:2型糖尿病患者质子泵抑制剂、肾病和心血管疾病有何关系?
2017-06-10 MedSci MedSci原创
由此可见,PPIs的使用与2型糖尿病患者经uACR评估的血管内皮功能持续的不利影响无关。然而,开始服用PPI与肾病恶化以及5年CVD风险增加之间的相关性,具有潜在的临床意义。
越来越多的证据表明慢性质子泵抑制剂(PPI)治疗会产生一系列不良反应。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在评估PPI对2型糖尿病患者蛋白尿、肾功能和心血管疾病(CVD)风险的影响。
该研究是在城市居住社区进行的纵向观察性研究。研究参与者来自于纵向观察性弗里曼特尔糖尿病研究II期的2型糖尿病患者,这些参与者稳定地服用肾素-血管紧张素系统阻断剂治疗,并被分为一直未用PPI治疗组(1组,n=686),全程PPI治疗组(2组,n=174),开始定期的PPI治疗组(3组,n=109)或停止定期的PPI治疗组(4组,n=67),在两次评估间隔两年。该研究的主要观察指标为尿白蛋白肌酐(UACR)的变化值(Δ),估计的肾小球滤过率(eGFR)和经过验证的方程预测的5年心血管疾病风险。
研究人员发现各组间ΔuACR没有统计学差异(方差分析,P=0.36),但ΔeGFR有所差异(ANOVA,P=0.002),其中3组表现出比1组显著降低(调整后的Δ平均差异(95%可信区间)为-2.7(-4.5至-0.8)毫升/分钟/1.73平方米)P=0.005)。Δ5年的CVD风险表现出了类似的模式(方差分析,P<0.001),其中3组比1组有更大的增加(调整后的Δ平均差异(95%可信区间)为1.7(0.6-2.8)%;P=0.002)。
由此可见,PPIs的使用与2型糖尿病患者经uACR评估的血管内皮功能持续的不利影响无关。然而,开始服用PPI与肾病恶化以及5年CVD风险增加之间的相关性,具有潜在的临床意义。
原始出处:
Timothy M E Davis,et al. Proton pump inhibitors, nephropathy and cardiovascular disease in type 2 diabetes: The Fremantle Diabetes Study. J Clin Endocrinol Metab. 2017. https://doi.org/10.1210/jc.2017-00354
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCE#
62
#质子泵#
66
#抑制剂#
74
#JCEM#
77
学习了谢谢分享
89
学习了不少事情!
123
#2型糖尿病患者#
93
#糖尿病患者#
54
#血管疾病#
83
学习啦,谢谢分享
126