PLoS One:精浆增强子宫颈癌细胞增殖以及肿瘤生长
2012-04-10 Deepblue 生物谷
在撒哈拉南部非洲,宫颈癌是一种主要引起妇女死因的癌症。广泛的证据表明,宫颈癌及其癌前病变是由人乳头瘤病毒(HPV)的感染引起。虽然绝大多数的HPV的感染是自然感染的,根除感染细胞的失败被表明会促进病毒存留以及肿瘤发生。 紧跟着致瘤性转化,通过直接或者是体循环的方式暴露在炎症因子中时,可能会增强宫颈上皮细胞疾病的发展。总所周知,精浆(SP) 包含了大量的炎症介质,它们都被鉴定为肿瘤生长有关的调节因
在撒哈拉南部非洲,宫颈癌是一种主要引起妇女死因的癌症。广泛的证据表明,宫颈癌及其癌前病变是由人乳头瘤病毒(HPV)的感染引起。虽然绝大多数的HPV的感染是自然感染的,根除感染细胞的失败被表明会促进病毒存留以及肿瘤发生。
紧跟着致瘤性转化,通过直接或者是体循环的方式暴露在炎症因子中时,可能会增强宫颈上皮细胞疾病的发展。总所周知,精浆(SP) 包含了大量的炎症介质,它们都被鉴定为肿瘤生长有关的调节因子。近日,来自南非开普顿大学的Arieh A. Katz等人研究了开展了一项有意义的研究,即研究精浆在调节宫颈上皮细胞生长和肿瘤发生中的作用。研究发现,精浆可以明显增强子宫颈癌细胞增殖以及肿瘤生长。相关研究发表在3月19号美国《公共科学图书馆·综合》(PLoS One)上。
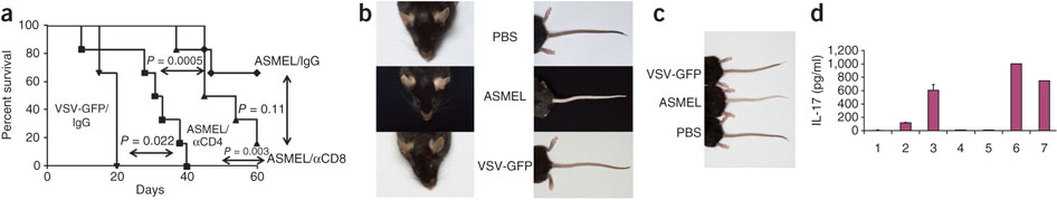
本次研究Arieh A. Katz利用了海拉细宫颈癌细胞,结果发现精浆(SP)引起了细胞内炎性酶,前列腺素内过氧化物合酶(PTGS1和PTGS2),IL-1及IL-11,血管内皮生长因子A(VEGF-A)的表达。为了研究在活体内精浆对肿瘤细胞生长的作用,他们异种移植海拉细胞于裸鼠的背部侧面皮下。研究发现,SP可以快速而明显的提高肿瘤生长率以及增大海拉细胞在裸鼠中的大小。检测发现,SP引起了体内的PTGS酶,细胞因子以及VEGF-A的表达。进一步研究发现,SP增大了这些裸鼠的血管。
结果表明,精浆确实增强子宫颈癌细胞增殖以及肿瘤生长。另外,SP引起的细胞因子的产生,VEGF-A的表达以及细胞增殖被PTGS通路所调节。(生物谷Deepblue编译)

doi: 10.1371/journal.pone.0033848
PMC:
PMID:
Seminal Plasma Enhances Cervical Adenocarcinoma Cell Proliferation and Tumour Growth In Vivo
Jason R. Sutherland, Kurt J. Sales, Henry N. Jabbour, Arieh A. Katzl.
Cervical cancer is one of the leading causes of cancer-related death in women in sub-Saharan Africa. Extensive evidence has shown that cervical cancer and its precursor lesions are caused by Human papillomavirus (HPV) infection. Although the vast majority of HPV infections are naturally resolved, failure to eradicate infected cells has been shown to promote viral persistence and tumorigenesis.Furthermore, following neoplastic transformation, exposure of cervical epithelial cells to inflammatory mediators either directly or via the systemic circulation may enhance progression of the disease. It is well recognised that seminal plasma contains an abundance of inflammatory mediators, which are identified as regulators of tumour growth. Here we investigated the role of seminal plasma in regulating neoplastic cervical epithelial cell growth and tumorigenesis.Using HeLa cervical adenocarcinoma cells, we found that seminal plasma (SP) induced the expression of the inflammatory enzymes, prostaglandin endoperoxide synthase (PTGS1 and PTGS2), cytokines interleukin (IL) -6, and -11 and vascular endothelial growth factor-A(VEGF-A). To investigate the role of SP on tumour cell growth in vivo, we xenografted HeLa cells subcutaneously into the dorsal flank of nude mice.Intra-peritoneal administration of SP rapidly and significantly enhanced the tumour growth rate and size of HeLa cell xenografts in nude mice. As observed in vitro, we found that SP induced expression of inflammatory PTGS enzymes, cytokines and VEGF-A in vivo. Furthermore we found that SP enhances blood vessel size in HeLa cell xenografts. Finally we show that SP-induced cytokine production, VEGF-A expression and cell proliferation are mediated via the induction of the inflammatory PTGS pathway.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#增强子#
65
#子宫颈#
67
#Plos one#
59
#癌细胞增殖#
66
#癌细胞#
62
#子宫颈癌#
92
#宫颈#
84
#细胞增殖#
67