J Urol:18F-DCFPyL-PET/CT可准确检出前列腺癌转移并定位转移灶
2021-03-01 MedSci原创 MedSci原创
18F-DCFPyL-PET/CT可准确检出前列腺癌转移并定位转移灶
目前常规的影像学方法,包括增强CT、MRI和99mTc-亚甲基二膦酸盐(MDP)骨成像,都不是检测不同状态的转移性前列腺癌(PCa)转移部位的理想方法。PSMA靶向PET/CT有望提高前列腺癌的检出和定位。
OSPREY是一项前瞻性试验,旨在确定18F-DCFPyL-PET/CT在检测转移性前列腺癌部位的诊断表现。
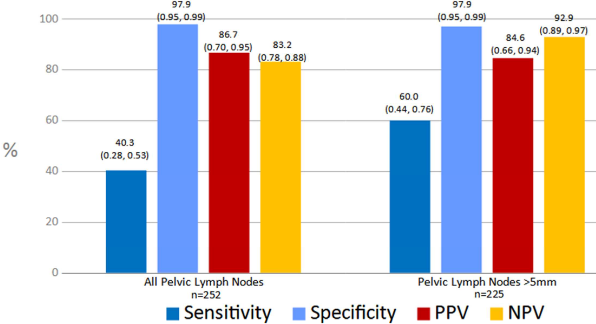
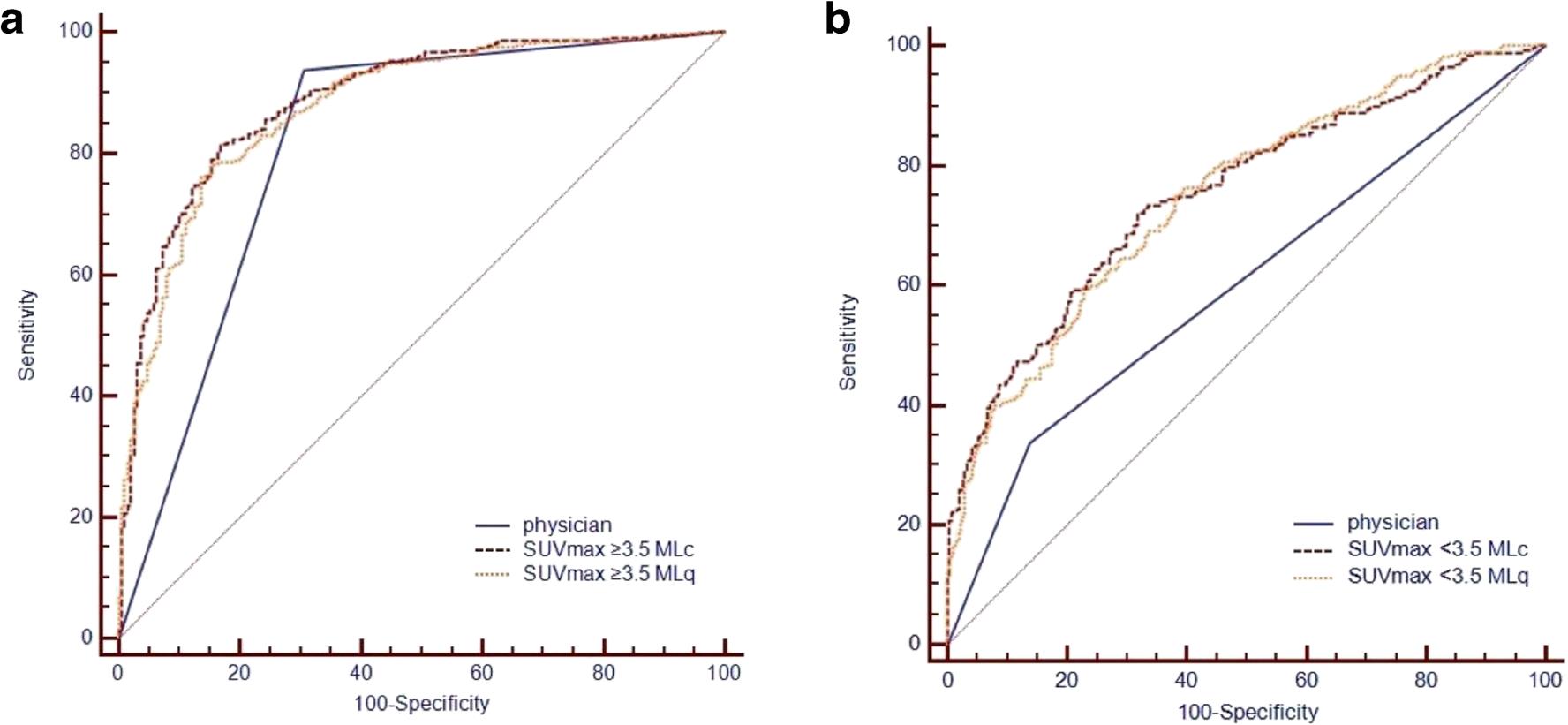
两组患者接受18F-DCFPyL-PET/CT检查:A组纳入接受根治性前列腺切除和盆腔淋巴结清扫术的高危PCa患者;B组纳入采用常规影像检查的怀疑复发/转移的前PCa患者。三个不知分组情况的中心的研究员对18F-DCFPyL-PET/CT扫描结果进行评估。18F-DCFPyL-PET/CT的诊断表现以影像学结果为依据,并与组织病理结果进行比较。在A组中,评估了盆腔淋巴结病变(特异性和敏感性作为共同的主要终点)和盆腔外转移。在B组中,评估了活检病灶检出PCa的敏感性、阳性预测值(PPV)及阴性预测值(NPV)。
共纳入385例患者。在A组(252个可评估对象)中,18F-DCFPyL-PET/CT检测盆腔淋巴结转移的特异性中位数为97.9%(95%CI:94.5%~99.4%)、敏感性中位数为40.3%(28.1%~52.5%,未达到预定终点);PPV中位数为86.7%(69.7%~95.3%)和NPV中位数为83.2%(78.2%~88.1%)。
在B组(n=93,中位PSA为11.3 ng/mL)中,对前列腺外病变的检出敏感度为95.8%(87.8%~99.0%),PPV为81.9%(73.7%~90.2%)。
综上所述,PSMA靶向PET/CT检出转移性前列腺癌的特异性达到预定的主要终点,但敏感性未达到。在两组患者人群中观察到的高PPV表明,18F-DCFPyL阳性病灶后可代表该疾病,支持18F-DCFPyL-PET/CT对有淋巴结或远处转移的高危PCa患者进行分期的潜在效用,并能可靠地检出疑似转移性PCa的转移部位。
原始出处:
Pienta Kenneth J,Gorin Michael A,Rowe Steven P et al. A Phase 2/3 Prospective Multicenter Study of the Diagnostic Accuracy of Prostate-Specific Membrane Antigen PET/CT with 18F-DCFPyL in Prostate Cancer Patients (OSPREY). J Urol, 2021: 101097JU0000000000001698.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
83
#DCF#
119
#转移灶#
112
#PET/CT#
120
#PET#
92
#癌转移#
123
可准确检出前列腺转移并定位转移灶
128
前列腺癌相关研究,学习了,谢谢梅斯
140
好文章!
182
目前常规的影像学方法,包括增强CT、MRI和99mTc-亚甲基二膦酸盐(MDP)骨成像,都不是检测不同状态的转移性前列腺癌(PCa)转移部位的理想方法。PSMA靶向PET/CT有望提高前列腺癌的检出和定位。
140