JACC:经导管二尖瓣置换术的可行性研究
2018-01-02 MedSci MedSci原创
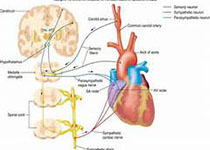
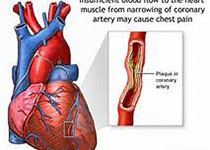
经导管二尖瓣置换术(TMVR)是一种具有潜力的治疗重度二尖瓣反流病人的手术方法,然而其可行性尚有待明确。本研究在14个临床研究中心招募了50例重度二尖瓣反流伴高危因素的患者(平均年龄为73 ± 9岁,男性占58%),并对所有参与者实施了经导管二尖瓣置换术。患者术前的胸外科协会平均评分为6.4 ± 5.5%,86%患者的纽约心功能评级为III或IV级,平均左室射血分数为43 ± 12%。人工瓣膜成功
经导管二尖瓣置换术(TMVR)是一种具有潜力的治疗重度二尖瓣反流病人的手术方法,然而其可行性尚有待明确。本研究在14个临床研究中心招募了50例重度二尖瓣反流伴高危因素的患者(平均年龄为73 ± 9岁,男性占58%),并对所有参与者实施了经导管二尖瓣置换术。患者术前的胸外科协会平均评分为6.4 ± 5.5%,86%患者的纽约心功能评级为III或IV级,平均左室射血分数为43 ± 12%。人工瓣膜成功在48例患者中植入,平均用时14min。术后30天死亡率为14%,无致残性卒中和反复介入治疗的发生。经过平均173天的随访,超声心动图结果显示在所有接受TMVR的患者中,二尖瓣反流均为轻度或者无残留,心功能评级也有明显改善(79%患者的纽约心功能评级为I或II级,p < 0.0001)。研究结果显示,经导管二尖瓣置换术在严重的二尖瓣反流患者中是可行的。原始出处:Vinayak B et al.Early Experience With New Transcatheter Mitral Valve Replacement. JACC,2018 Jan.本文系梅斯医学(MedSci)原创编译
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#可行性#
89
#置换#
57
#经导管二尖瓣置换术#
171
#JACC#
94
#二尖瓣置换术#
87
一起学习学习
106
一起学习学习学习
131
#ACC#
75
#二尖瓣#
57
#经导管#
59