产前超声诊断胎儿膈下隔离肺1例
2018-10-29 吕白雪 姜镔 王学梅 中国医学影像技术
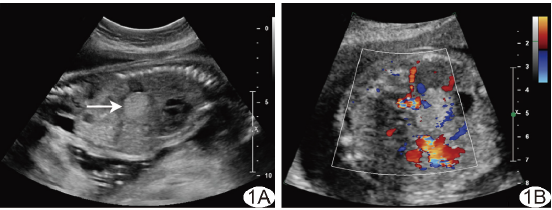
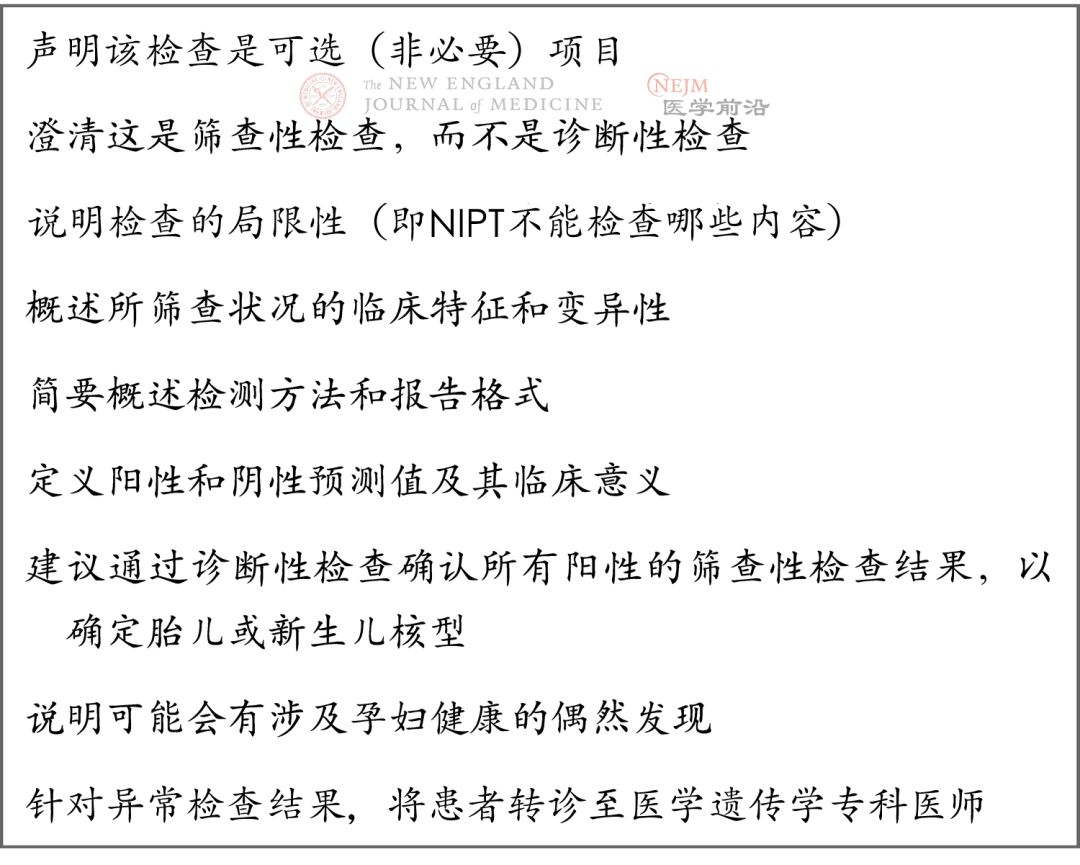
孕妇33岁,孕1产0,因“孕24+2周产前超声检查发现胎儿腹部包块”就诊,无家族遗传病史。超声检查显示胎儿左肾上方肾上腺区见大小约2.1 cm×1.7 cm×1.5 cm高回声包块,类圆形,内部回声均匀,边界清晰,与肾上腺分界清(图1A)。CDFI示高回声包块内部供血动脉起源于腹主动脉(图1B)。超声诊断为膈下隔离肺。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#产前超声#
89
#隔离肺#
71
谢谢分享,学习一下。
110
#产前#
61
#超声诊断#
78
#超声诊断#
66
学习了
0