Nature:发现新的肥胖标志物---神经降压素前体(pro-NT)
2016-05-14 MedSci MedSci原创
一项新的研究中,来自美国肯塔基大学、马萨诸塞大学和瑞典隆德大学的研究人员发现肥胖产生的一个潜在的新的生物标志物,而且该生物标志物也可能是预防和治疗肥胖的靶标。相关研究结果于2016年5月11日在线发表在Nature期刊上,论文标题为“An obligatory role for neurotensin in high-fat-diet-induced obesity”。神经降压素(neuroten

一项新的研究中,来自美国肯塔基大学、马萨诸塞大学和瑞典隆德大学的研究人员发现肥胖产生的一个潜在的新的生物标志物,而且该生物标志物也可能是预防和治疗肥胖的靶标。相关研究结果于2016年5月11日在线发表在Nature期刊上,论文标题为“An obligatory role for neurotensin in high-fat-diet-induced obesity”。
神经降压素(neurotensin, NT)是一种主要在胃肠道和中枢神经系统中产生的肽,是在脂肪摄入时释放出来的。它促进肠道脂肪酸吸收。之前的研究已证实NT也能够促进多种癌症的生长,而且增加的空腹pro-NT(NT前体激素)水平与心血管疾病和乳腺癌产生相关联。
在这项新的研究中,研究人员分析了来自马尔默饮食和癌症研究(Malmö Diet and Cancer Study)---一项基于人群的前瞻性流行病追踪研究(study cohort),涉及28,449名男性和女性,他们接受平均16.5±1.5年追踪研究---的数据。这一发现表明肥胖的和胰岛素抵抗的参与者具有显著提高的空腹pro-NT水平,而且相比对于空腹pro-NT水平最低的参与者而言,空腹pro-NT水平最高的非肥胖参与者患上肥胖的风险会加倍。
研究人员继续利用模式动物证实NT缺乏可预防与高脂肪摄入相关联的肥胖、胰岛素抵抗性和脂肪肝,因此鉴定出NT是在未来产生肥胖的一种潜在的早期标志物,也是这种疾病的一种新的治疗靶标。
论文通信作者、肯塔基大学马基癌症中心(Markey Cancer Center)主任Mark Evers博士说,“我们的发现重新确定了我们看待NT作用的方式。NT似乎是一种代谢上‘节俭’的肽,增加摄入的脂肪的吸收;然而,由于典型的西方饮食含有大量脂肪,NT也因能够促进肥胖和代谢病产生而发挥有害作用。”
此外,鉴于NT能够促进某些癌症生长,而且如今它也与肥胖相关联,Evers猜测增加的NT水平可能导致与肥胖相关联的某些癌症的较高发病率。基于这项研究的发现,肯塔基大学的未来研究将探究这种可能的关联性。
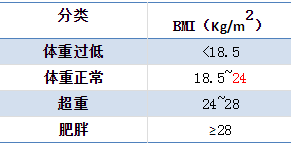
在全世界,17亿多人是超重的,即身体质量指数(BMI)高于25,或者是肥胖的,即BMI高于30。另外,每年250万死亡病例归因于肥胖带来的健康问题。
原始出处:
Jing Li, Jun Song, Yekaterina Y. Zaytseva, Yajuan Liu, Piotr Rychahou, Kai Jiang, Marlene E. Starr, Ji Tae Kim, Jennifer W. Harris, Frederique B. Yiannikouris, Wendy S. Katz, Peter M. Nilsson, Marju Orho-Melander, Jing Chen, Haining Zhu, Timothy Fahrenholz, Richard M. Higashi, Tianyan Gao, Andrew J. Morris, Lisa A. Cassis, Teresa W. -M. Fan, Heidi L. Weiss, Paul R. Dobner, Olle Melander, Jianhang Jia & B. Mark Evers. An obligatory role for neurotensin in high-fat-diet-induced obesity. doi:10.1038/nature17662
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
73
#Nat#
101
#降压#
65
#PRO#
62
生物标志物,未来有可能成为,治疗的靶点
139