颈清术中见PICC管异位于颈内静脉1例
2018-11-07 周竹云 刘向辉 孙卫革 口腔颌面外科杂志
目前晚期舌癌主要采用以手术为主的综合序列治疗(术前诱导化疗+手术治疗+放化疗),其中术前诱导化疗常规行PICC置管。现报道1例舌癌患者完成术前诱导化疗2个周期(PR)后,行手术治疗,当患侧行根治性颈部淋巴结清扫,剪断颈内静脉下端后,见两断端血管内均有PICC管,经及时妥善处理,术中成功将PICC管拔除,报道如下。
目前晚期舌癌主要采用以手术为主的综合序列治疗(术前诱导化疗+手术治疗+放化疗),其中术前诱导化疗常规行PICC置管。现报道1例舌癌患者完成术前诱导化疗2个周期(PR)后,行手术治疗,当患侧行根治性颈部淋巴结清扫,剪断颈内静脉下端后,见两断端血管内均有PICC管,经及时妥善处理,术中成功将PICC管拔除,报道如下。
1.资料和方法
1.1一般资料
患者男性,61岁,渐进性吞咽困难加重半年,来院就诊查体见舌根肿物(偏右侧),直径约2.0 cm,右颈动脉三角区可触及一肿大淋巴结,结节状,直径约3.0 cm,界限欠清,无活动度。给予切取活检,病理报告示:舌根鳞状细胞癌(低分化)。颌面颈部MRI示:右舌根部软组织肿块,伴右侧颈部多发肿大淋巴结,舌癌伴淋巴结转移可能。舌癌分期:T2N2aM0。
1.2方法
1.2.1术前诱导化疗
给予行PICC置管,采用60 cmPICC导管,置入长度为45 cm。经无菌操作置入导管后,常规胸部X片检查示:PICC管头端位于胸9椎体上缘水平。PICC管无颈内静脉异位。行TPF方案术前诱导化疗2个周期,期间患者未出现明显毒副反应。评估术前诱导化疗效果为PR。
1.2.2手术治疗
先行右侧根治性颈部淋巴结清扫术。术中游离颈内静脉下端后,于拟剪断处上下端分别用7、4、1号线三重结扎,遂剪断颈内静脉,见两断端血管断面内均有导管状物(图1)。
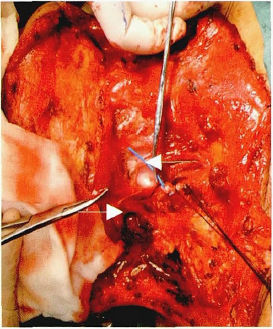
图1 颈内静脉内异位PICC管(白色箭头)
术中请巡回护士自患者右前臂PICC置管处向外抽动导管,见颈内静脉下端连同静脉内管状物随之向下移动,频率及动幅一致,再结合体外观察到的PICC管外形、颜色、管径和颈内静脉内导管比较,判断颈内静脉为异位的PICC管。用4号缝线分别于颈内静脉两断端处悬吊4针,以防止血管退缩,悬吊线下方颈内静脉用血管钳夹持,防止出血。保持悬吊颈内静脉上下端,松开血管钳的同时,台下巡回护士自右前臂成功缓慢抽出PICC管,颈内静脉导管去除,血管钳夹闭颈内静脉下端,并用7、4、1号线三重结扎。同样成功取出上端颈内静脉内的PICC管末端。后续手术顺利完成。
2.讨论
2.1经验总结
目前口腔颌面头颈恶性肿瘤治疗时常先给予诱导化疗,通过控制癌细胞播散转移,改变癌细胞的辐射剂量效应曲线,干扰细胞动力学,以缩小肿瘤体积,减少副作用,便于手术操作并降低癌细胞活性。经术前化疗达到预期效果后,再行手术治疗。口腔颌面部恶性肿瘤主要经颈部淋巴结转移,所以手术常涉及颈内静脉的处理。在未知的情况下,出现PICC导管异位颈内静脉,则明显增加了手术中出血的风险,严重影响了手术的安全性。
根据本病例的处理经验,此刻应冷静,仔细的游离颈内静脉两断端,静脉断口处给予缝线悬吊,以确保去除PICC管时颈内静脉不会随之移动,同时保持管腔通畅。在拔除PICC管的后,血管钳立刻夹闭颈内静脉,并给予结扎。
2.2预防措施
PICC是目前首选的静脉化疗途径,与传统的静脉给药和锁骨下深静脉置管术相比,具有安全、可靠、留置时间长,并发症少的优点。目前也广泛应用于口腔颌面头颈肿瘤的术前诱导化疗中。PICC置管时常见导管会异位至颈内静脉中,若置管时未发现异位情况,后续化疗时可致后组颅神经损伤等并发症,表现为吞咽困难、饮水呛咳、声音嘶哑、咽反射减弱或消失等。为了避免PICC管异位的情况出现,目前常规PICC置管后,立刻行胸部X片检查,明确PICC管的位置,若发现异位,则立即处理使导管到达预定位置。
本例患者经PICC置管后,胸部X片检查见导管已到达预期位置。随后的术前诱导化疗期间,患者也未出现明显后组颅神经损伤症状,但在之后的手术中发现,PICC管已异位至颈内静脉内。提示PICC置管时虽已到达预期位置,之后仍有可能出现异位。治疗期间PICC管是否出现异位,不可单凭患者有无后组颅神经损伤症状及其他临床表现判断。需何时复查PICC管有无异位,暂无明确报道。笔者认为携带PICC管的口腔颌面恶性肿瘤患者在手术前需复查胸片,排除PICC管异位至颈内静脉的情况,以确保手术安全。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#颈内静脉#
77
#静脉#
54
#PICC管#
72
#PICC#
68
#ICC#
69