Nature Methods:2016 值得关注的 8 大生物医药技术
2016-01-08 张巨岩 新智元
《Nature Methods》是Nature旗下最重要子刊之一,也是方法论领域的权威刊物,其影响因子自从2004年创刊开始就一路飙升,在2014年已经达到32.072。这个月更期刊的受众是学术和产业界的从事实验工作的研究人员。它旨在为研究人员提供新工具来方便研究,Nature Methods强调方法的实用性和即时性。 《Nature Methods》选出了 2016 您最值得关注的
《Nature Methods》是Nature旗下最重要子刊之一,也是方法论领域的权威刊物,其影响因子自从2004年创刊开始就一路飙升,在2014年已经达到32.072。这个月更期刊的受众是学术和产业界的从事实验工作的研究人员。它旨在为研究人员提供新工具来方便研究,Nature Methods强调方法的实用性和即时性。
《Nature Methods》选出了 2016 您最值得关注的八项技术:细胞内蛋白标记(Protein labeling in cells)、细胞核结构(Unraveling nuclear architecture)、动态蛋白质结构(Protein structure through time)、精准光遗传学(Precision optogenetics)、高度复合成像(Highly multiplexed imaging)、深度学习(Deep learning)、蛋白定位亚细胞图谱(Subcellular maps)、综合单细胞图谱(Integrated single-cell profiles)。另外,《Nature Methods》也选出了 2015 年最受关注技术成果:单颗粒冷冻电镜。
2016年值得关注的方法
深度学习(Deep learning)新的计算工具从大量的序列数据集中学习复杂模式。

机器学习中,一个功能强大方法可以让计算机解决感知问题,如图像和语音识别技术越来越多地进入生物学。这些深度学习方法,如深度人工神经网络,使用多个处理层从海量数据中发现模式和结构。每一层都用将前一层从数据中学到的概念作为基础;级别越高,所学的概念越抽象。深度学习不依赖于预先数据处理并自动地提取特征。举一个简单的例子,用于理解形状的深度神经网络在第一层中学习识别简单的边,然后在后续层中识别由那些边组成的更复杂的形状。深度学习的层数并没有硬性规定,但多数专家认为,至少需要两层。
最近的例子展示了深度学习的力量——它可以从基因组DNA序列中找到调控特点:DeepSEA(Nat. Methods 12, 931–934, 2015)将基因组序列作为输入,数据来源是如ENCODE和Epigenomics Roadmap这样的大型数据库,进而预测单核苷酸变异对调节区域——如DNA酶超敏感位点,转录因子结合位点和组蛋白标记——的影响。Basset(bioRxiv,DOI:10.1101 / 028399,2015)使用类似的深度神经网络预测单核苷酸多态性在染色体上的影响。 DeepBind(Nat. Biotechnol. 33, 831–838, 2015)用深度学习发现RNA和DNA上的蛋白结合位点,并预测突变的影响。
深度学习在大数据的背景下是非常有价值的,因为它从大量数据中提取出高层次的信息。它在基因组分析的逐步应用会解决一些最初的挑战,如由于稀少训练数据的相关性而产生的过拟合问题,还有高计算成本问题。学术领域和新兴公司的(如Deep Genomics,2015年7月22日成立)的研究人员将越来越多地应用深度学习来进行基因组分析和精确预测药物。当前目标是预测基因变异对细胞调节总体情况和疾病发展的影响,不管这种变异是自然状态下发生的还是由于基因组编辑引入的 。
细胞内蛋白标记(Protein labeling in cells)更好的蛋白标记技术会提高成像。
荧光化学染料相对较小,具有良好的光物理性质还有多种颜色,这使它们成为可取代荧光蛋白的备选方案。研究人员正积极开发在活细胞中用染料标记蛋白的工具。为了实用,让染料浸染蛋白的方法必须支持蛋白质的特异性标记。在这方面,已经存在一些工具,如SNAP和Halo标签、Flash和ReAsH和组氨酸标记。这些工具包括了一些标记靶蛋白并与染料特异性结合的小分子蛋白或肽。一种替代方法是在翻译过程中,将非天然氨基酸加入到蛋白质中;这里所讲的非天然氨基酸或者是荧光的,或者可以通过“点击化学”制成荧光。
虽然这些方法日益普及,它们也有如复合成像方法用途有限问题,低标记效率问题和染料能穿过活细胞膜的数量和质量问题。这种染料的研发是一个活跃的研究领域。今后的工作无疑将会提高标记效率,这将有助于增强定量成像;提高现有染料质量,增加复用次数,减少必要的成像光剂量;还可能揭示蛋白质全新的标记方法。
特异性蛋白标记也将提高某些活细胞的超高分辨率成像。随着解析能力接近几十纳米,标记方法脱颖而出。例如,用抗体标记会增加结构精度,而且使用二次抗体会更加精确。还有一种替代方案,研究人员正在开发纳米抗体,它是更小的用于标记的单链抗体。
细胞核结构(Unraveling nuclear architecture)我们需要新方法来支持高分辨率和高吞吐量地观察3D染色质结构的动态变化。

房地产的口头禅——“位置比其他都重要”——同样也适用于哺乳动物的基因组。基因调控取决于染色质的构建和其在细胞核内的三维调控元件。在特定位点或全基因组范围内的染色质构象捕获(capture chromatin conformation,3C)是一种窥探基因组复杂结构的方式。但想要真正理解这个3D结构,它如何随时间演变,以及它对疾病的作用,还需要新方法。 由3C衍生出的技术通常依赖染色质相互作用位点的交联,还依赖在扩增和测序之前这些位点的连接反应。这些步骤限制了该方法的吞吐量,使其更支持顺式的相互作用,而非反式。最近在复用—顺式相互作用方向上的进步包含两个连续捕获步骤,它提高了吞吐量和分辨率,支持弱相互作用和强相互作用的相对定量,还能解释它们各自的生理作用。
为了让科学家们充分理解细胞核组织的动态变化,应该将基于群体的模型和个体每个细胞的高分辨率数据结合起来。这将需要多学科方法来汇集基因组学,生物物理学和成像学的精髓。最近由美国卫生国家研究院资助的4D Nucleome计划,是一项倡议,旨在结合这种专业技能并联合大型数据库来比对基因组结构,应用高分辨率成像并研究细胞核内区室。其目标在于改良工具,这包括改进针对单细胞核小体实验成像分辨率的实验计算方法,和让基因组折叠的可视化的实验计算方法。
一旦细胞核结构的比对变成一个更常规的定量过程,我们将能更好地确定和预测的突变对基因调节和作用机制的影响——是与疾病有关,还是在基因组编辑的过程中引入。我们甚至能够特异性改变基因组结构,进而在细胞中实现预期的改动。
动态蛋白质结构(Protein structure through time)时间分辨晶体学的进步让我们可以追踪更多蛋白结构的快速改变。
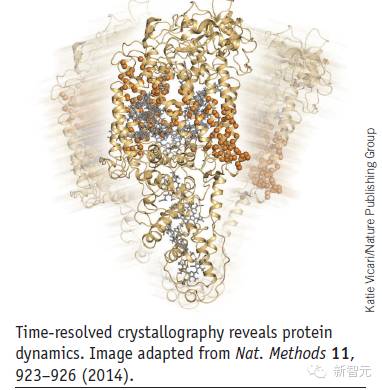
蛋白质的静态结构为生物学家提供了更多发现其功能的机会,但研究人员可以通过观察蛋白质的变化来获得更深入的见解。然而,检测稍纵即逝的中间构象状态是一个很难克服的实验挑战。
研究蛋白质动力学的一种方法是时间分辨X射线晶体学(TRX)。在TRX的研究中,一个激光脉冲用以触发反应,然后X射线“探针”脉冲被施加来收集反应过程中的一系列衍射图案。过去在执行这种实验需要高度专业的同步辐射源。这些仪器具有约100皮秒“速度限制”,这不无法支持变化很快的构象可视化。但现在,最新进展——超快X射线自由电子激光(XFELs)使其成为可能,它能提供飞秒级的时间分辨率,让研究人员可以解决任何其他方法无法检测到的非常迅速的结构变化。
例如,在2014年,研究人员使用XFEL为基础的TRX来追踪处于光催化水分解过程中的光系统II的快速构象变化,实验的分辨率达到5.5埃(Nature 513,261-265,2014)。随后,一个团队也用了这种方法来研究光敏蛋白的光周期,在1.6埃分辨率下找到了反应中间体(Science 346,1242–1246,2014)。2015年,另一组人利用超快XFEL脉冲来追踪肌红蛋白的结构变化(Science,350,445-450,2015)。鉴于XFEL仪器在全世界范围数量较少,这种实验的普及范围相比TRX实验并不广。因此,可用于TRX实验数据收集的任何标准的同步辐射源,将更有利于进入实验室,因而是一个更受欢迎的发展(Nat.Methods 11,1131—1134,2014)。虽然该技术的时间分辨率还没有被证明与XFEL一样好用,但未来的发展可能会改进这种方法。看到TRX技术被广泛的使用一定会很有趣,特别是看到研究人员如何调试方法来研究非光激发的蛋白质的超快反应。
精准光遗传学(Precision optogenetics)细胞水平上对神经元的光遗传学控制在神经微电路的解析领域中很有前景。

2015年是将channelrhodopsin2(ChR2)引入到神经科学的10周年。ChR2已被证明是一种强大的工具,不仅能用于刺激神经元,而且也能推动其他光遗传学工具的研发。通常情况下,这些工具能够用于多个领域,尤其适用于遗传定义神经元的表达。但要想对神经回路有更详细的了解,模式照明方案就可以派上用场,这些方案可以让人们操纵特定物种的神经元亚群的活性。
所需的照射样式可以以不同的方式产生。用快速扫描镜照明是一种方式,由计算机产生的全息图案可以通过空间光调制器来产生。此外,照明方案需要与神经活动光学输出结合起来,这往往需要用到光遗传活化。这并不容易且需要优化,这是由于光遗传学活化剂和活动传感器之间的光学交流干扰。
最近推出的一些方法为研究人员提供了各种战略。通过将一束有两个光子的激光聚焦到胞体的大小并在快速扫描镜(Nat. Neurosci. 17, 1816–1824, 2014)的帮助下在不同的神经元之间的切换来实现两个神经元几乎同时的照明。人们也可以通过将一个双光子束分成多个子束,并用空间光调制器将它们定位到感兴趣的神经元上(Nat. Methods 12, 140–146, 2015)来实现同时照明。在这两项研究中,红移光遗传执行器(C1V1)的使用减少了检测神经活动的绿色钙指示器的光干扰。在无行为动物中,纤维内窥镜(fiberscopes)可以通过传递单光子照明实现相同的模式((Neuron 84,1157–1169,2014)。
细胞水平的光遗传学将继续推动我们对神经亚群多样性和功能的理解。然而,这些方法只能在单一的二维平面上刺激神经元,然而神经元的通信和工作却是在大脑的三维环境中进行的。将这些光刺激的方法提升到三维很可能会开辟探测神经元新的可能性。
高度复合成像(Highly multiplexed imaging)单细胞多靶点成像方法打破了颜色障碍。
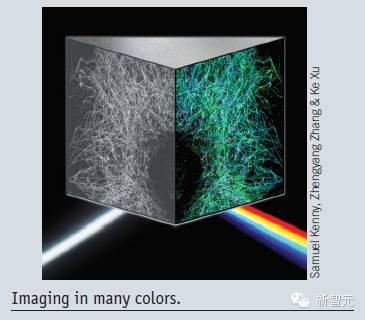
可视化生物结构的一个主要障碍是荧光光谱的重叠。这种“颜色障碍”实际上将大部分实验限制到只能进行三或四个靶点的测试。但是,如果我们能看到许多颜色的细胞呢?复合成像可以在更有意义的情景中观察结构,并让我们更好分析多成分复合物如何在细胞中形成和改变。它有望改变我们对生物学过程的理解。
现在有几种策略可以解决复合成像问题。开发者正在设计更好的探针;这其中包括了横跨可见光和更多的色彩范围的探针,以及如细胞内微型激光器这样的探针(Nat. Photonics 9, 572–576, 2015; Nano Lett. 15, 5647–5652, 2015),这类探针有非常窄的色谱,因而彼此区分比较容易。这些探针的改进可以让标准的显微镜呈现更好的复合图像。
研究人员还开发光学设备来检测重叠荧光。例如,Ke Xu和他的同事开发了SR-STORM显微镜,该款显微镜通过真彩高分辨率成像来测量标记分子的位置和光谱(Nat. Methods 12, 935–938, 2015)。有了这样的方法,即使高光谱重叠的荧光也可以被很容易地识别,这打开了复合成像的大门。
高度复合免疫荧光成像方法也在不断出现。在这些方法中,用抗体标记一些靶点并成像,接着,这些探针被漂白或剥离,然后对不同的靶点重复同样的标记过程。这就通过多次步骤建立高度复合颜色的图像。
一个相关的策略已经用于高度复合转录组成像中,在这个方法中,每个转录产物通过一个独特的条码识别(Nat. Methods 11,360–361,2014; Science 348, aaa6090, 2015)。在zhuang实验室MERFISH方法中,成千上万的转录物只用一个颜色成像。
虽然这些方法都很强大,活细胞复合成像仍然需要改进方法。 活体细胞方法和固定细胞方法有相同的问题,但它们也有其他挑战,如有用的荧光染料和探针的范围较小、需要快速获取图像,以及对光线的敏感。实现大规模复合成像的方法会继续被研发,以推动对生物过程的研究。
蛋白定位亚细胞图谱(Subcellular maps)系统绘制蛋白质在细胞中分布的方法也在不断发展。
人类几个世纪以来一直在绘制地球,海洋和天空,但最近几十年,我们才扩大范围,从分子水平上探索细胞。
不仅仅是细胞质,细胞的结构也是严密的。它们被区分为细胞器和有特定分子组成和物理性质的结构域,并且它们也是动态的,任一时间段内进入和离开它们的分子数量是稳定的。毫无疑问,细胞过程依赖于其结构:细胞分泌,需要通过一系列的膜结构才能发生;许多信号过程是通过分子支架来完成的。甚至基因表达也与基因组的空间结构有错综复杂的联系。尽管细胞结构和蛋白定位从细胞生物学出现开始就一直是研究热点,用于绘制整个细胞的蛋白分布系统分子地图的技术方法仍在发展。
在早期的工作中,人们先进行细胞分馏,随后对蛋白质位置进行生化分析,这其中主要用了质谱方法(Cell 125,187-199,2006)。在系统中使用Workhorse方法,如以抗体为基础的免疫组化方法,以产生亚细胞图谱。还有遗传编码工具,如抗坏血酸过氧化物酶和生物素连接酶,都可以用在生物素化分析方法中,还有捕获和质谱法,用以确定在细胞特定位置有哪些蛋白(Science 339, 1328–1331, 2013; J. Cell Biol. 196, 801–810, 2012)。这些工具一直在被改进(Nat. Methods 12, 51–54, 2015),并开始在亚细胞图谱实验中应用((Proc. Natl. Acad. Sci. USA 112,12093–12098, 2015)。
虽然蛋白质位置的亚细胞地图会让我们看到前所未有的图像,但是蛋白质只是组成这种图像的为数不多的一种分子类型。然而,在对细胞的探索中,蛋白质图谱肯定是开始的地方。
综合单细胞图谱(Integrated single-cell profiles)单细胞的综合分子图谱将为基因调控和异质性提供关于其机制的见解。
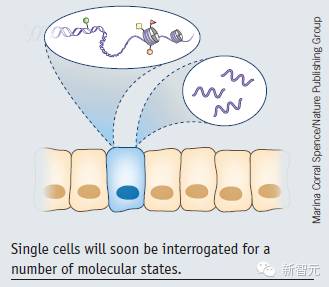
就像一副新眼镜,单细胞测序正被越来越多的科学家使用来重新审视他们的研究。在细胞的水平上检查组织可以深入了解异质性,还可以让研究人员能够直接定义细胞,这其中包括通过比较分子状态来定义新细胞类型。单细胞DNA和RNA测序方法日趋完善,并且近期有很多表观遗传学方法达到了单细胞的里程碑。我们期待着表观遗传分析更进一步,以及出现从同一细胞中提取多个图谱的新方法。
在单个细胞中进行RNA测序已经可以很强大而常见了,而且也有可能大规模使用;可以用它来得到表型进而推断细胞的身份和功能。现在,研究单细胞基因调控的方法包括了对DNA甲基化,进入染色质,组蛋白修饰和染色体结构的研究。虽然成就是非凡的,这些方法大多数将受益于更大的基因组覆盖范围和更清晰的信号。解析问题还需要解决;高技术的噪音,由于欠采样和生物变化(例如,来自细胞周期的不同,批次效应和生化随机性)而造成的数据稀疏性问题是其中的一些挑战。
从大量的表观遗传学数据中找出机制或因果关系被证明很难。许多数据类型是相关,并在许多细胞群中与基因表达有复杂的关系。提取表观遗传学特征和相同细胞的RNA有可能是找到“表观遗传状态如何影响基因表达,或者RNA如何响应表观遗传学的变化”的更直接的方法。此外,基因表达原则上可以用于将细胞分配到亚种类中,用其他论文中的表观遗传学特征进行单细胞RNA分析比对——例如,在一个实验中的DNA甲基化过程和另一个中的DNA可进入性过程——可以识别每个亚群中表观遗传特征的关系,以及它们在基因表达的潜在作用。
单细胞方法对干细胞生物学的研究、发展,还有对组织异质性的研究非常重要。有了足够的样本,就有可能解决表观遗传如何影响各个位点的基因表达。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
85
这篇文章有一定深度
161
是一篇不错的文章
164
#MET#
69
#医药#
65
牛
141
牛掰,
157
牛掰,
111
厉害
92
终于开始有点明白医学上为什么有那么多解决不了的问题和困境了
92