Inflamm Bowel Dis:缓解期炎症性肠病患者的腹痛、腹泻症状可能与肠道微生物无关
2018-08-20 鸟爪爪 IBD学术情报官
炎症性肠病(IBD)是一种慢性胃肠道炎性疾病,肠道免疫功能混乱和异常是主要特征。
既往的观点和实践
肠易激综合征(IBS)是一种胃肠道功能紊乱性疾病,持续或间歇发作,表现为腹痛、腹胀、排便习惯和(或)大便性状改变,但患者并没有明显的系统性炎症反应。
从发病机制上看,上述两个疾病存在非常显著的差异,但IBD和IBS患者常表现为相似的临床症状,例如:腹痛、腹泻等。尤其是在IBD患者的炎症缓解期,常出现IBS相似症症状,难以判断是否与肠道炎症有关。
据统计,在缓解期高达35%的IBD患者存在符合肠易激综合征(IBS)的症状。因此,IBD患者在炎症缓解期出现类似IBS的症状,判断腹痛、腹泻症状与炎症的关系,就显得非常重要。
之前有研究显示,肠道微生物的异常与炎性肠病(IBD)和肠易激综合征(IBS)的发病机理均相关,提示这两种疾病可能具有共同的病因。
目前已经有部分证据支持上述观点。
首先,传统IBD抗炎药物,在炎症负担有限的IBD患者中疗效较差。
其次,粪钙卫蛋白等生物标志物的应用,证实了确实有部分IBD患者在炎症静息的时期,仍然经历着持续的腹部症状,严重影响生活质量。
目前,越来越多的研究,开始关注这类患者的疾病管理策略,尤其是针对肠道微生物的研究。
面临的问题
尽管有很多IBD患者都在炎症静息经历了腹部症状,但针对这类患者的研究数据非常有限。
由于处于炎症静息期,这类IBD患者不会被纳入临床研究,更加剧了数据缺乏的情况。
既然肠道微生物异常对IBD和IBS患者都有影响,因此有理由怀疑,静息IBD患者出现腹痛、腹泻等IBS型症状,与肠道微生物的改变有关,但目前还无法证实上述猜想。
这项研究有什么新发现
这是一项横断面研究,共纳入270例IBD患者,通过临床疾病活动指数(CDAI)、粪钙卫蛋白水平、IBS诊断标准(罗马III),将IBD患者分为4组:
1、患者存在IBS症状
2、症状和疾病活动处于静息期
3、患者存在隐匿性炎症活动
4、患者处于炎症活动期
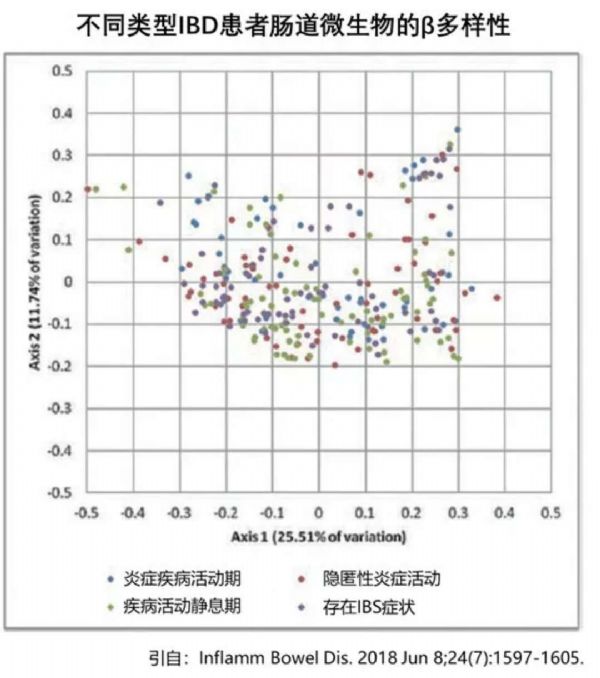
对所有进行A16SrRNA微生物组分析,确定不同类型患者是否存在肠道菌群的丰度差异。尤其对比存在IBS症状的患者,与其他3组患者相比菌群多样性是否存在任何差异。
研究结果显示,在所有270例患者中,25.9%(70例)存在IBS症状,30.0%(81例)为静息性IBD,24.4%(66例)存在隐匿性炎症,19.6%(53例)处于炎症活动期。
对肠道菌群的分析结果显示,存在IBS症状的患者,肠道放线菌的丰度没有显着增加,而且在任何分类水平,与其他3组患者都不存在肠道菌群类别的差异。
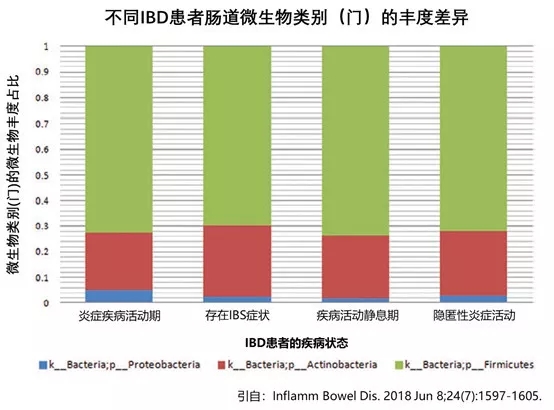
因此,这项研究初步显示,肠道菌群的变化可能并不影响IBD患者是否出现IBS症状。
启示和影响
这项研究发现,无论在任何肠道菌群分类水平上进行分析,存在IBS症状的IBD患者与静息疾病、隐匿性炎症、活动性炎症的患者,都没有观察到显著差异。
IBD患者本质上是一个复杂的人群,相互之间存在很大差异。目前已知很多因素有可能影响患者的肠道微生物,例如:既往手术、病变部位和表型、年龄、体重和药物,但这些因素交织在一起使得对肠道微生物的影响异常复杂。
目前,已经有部分肠道菌群调节药物,开始用于肠易激综合征(IBS)的治疗。
但根据这项研究的结果,对于疾病缓解期出现腹痛、腹泻等IBS症状的IBD患者来说,单纯给予肠道菌群调节药物可能不一定有效。对这类患者腹部症状的管理策略,还需要进一步的研究。
目前已知,精神心理因素对IBS症状具有重要的影响。因此,对于处于缓解期的IBD患者,尽管炎症的问题得到解决,仍不应该忽略患者精神心理的负担和影响,以降低患者出现IBS症状的风险,使患者从炎症负担和腹部症状的方面,都能获得“缓解“”,从而提高生活质量。
因此,尽管肠道菌群干预(如粪菌移植)已经证明可用于部分IBD患者的治疗,但这类菌群干预疗法,目前可能仅适用于治疗炎症活动性的症状和疾病。
肠道菌群干预对于IBD患者炎症缓解期的腹部症状的意义和价值,还有待于进一步的研究和论证。
原始出处:
Shutkever O, Gracie D J, Young C, et al. No Significant Association Between the Fecal Microbiome and the Presence of Irritable Bowel Syndrome-type Symptoms in Patients with Quiescent Inflammatory Bowel Disease[J]. Inflammatory Bowel Diseases, 2018.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Bow#
55
#缓解期#
40
#LAM#
42
#微生物#
42
#Dis#
47
学习了
81
#腹痛#
35
#NFL#
39
#bowel#
44
#炎症性#
39