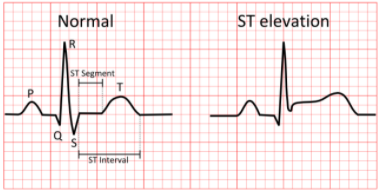
J INTERN MED:ST段抬高型心肌梗死患者入院时精氨酸酶1水平表达上调
2021-07-10 MedSci原创 MedSci原创
入院时精氨酸酶1的基因和蛋白表达显著增加表明精氨酸酶1在STEMI发生发展中发挥着重要作用。
ST段抬高型心肌梗死(STEMI)患者冠状动脉粥样硬化斑块破裂和心肌缺血再灌注损伤发生发展的潜在机制仍未明确。精氨酸酶1活性的增加导致一氧化氮(NO)的产生减少,由于产生NO的酶内皮NO合酶(eNOS)的解偶联导致活性氧产生增加。这将导致急性心肌梗死内皮功能障碍、斑块不稳定和对缺血再灌注损伤的易感性增加。
近日,内科学领域权威杂志Journal of Internal Medicine上发表一篇研究文章,该研究旨在评估STEMI患者精氨酸酶基因和蛋白质表达是否上调。
两个队列的STEMI患者被纳入。在第一个队列(n=51)中,研究人员测定了受试者精氨酸酶和NO合酶的表达以及精氨酸酶1蛋白水平,并将其与健康对照组(n=45)进行比较。在第二个队列(n=68)中,研究人员使用心脏磁共振成像确定了血浆精氨酸酶1水平和心肌梗死面积。
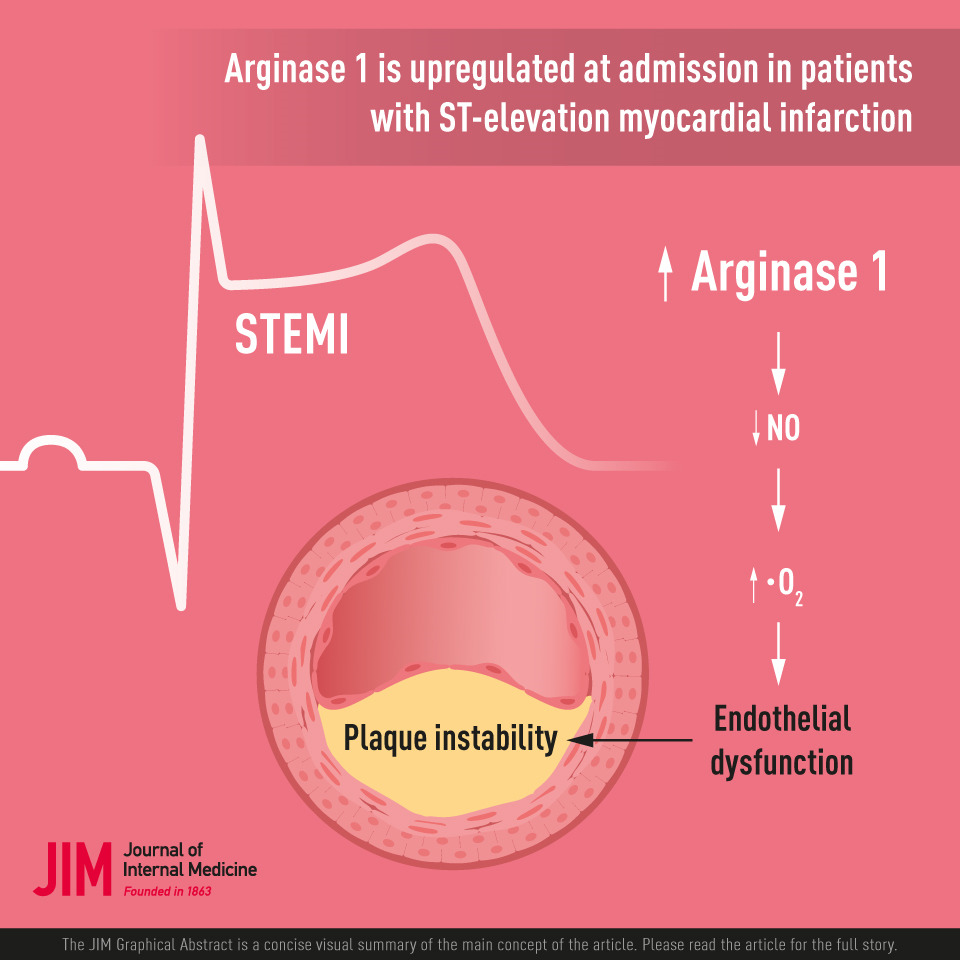
与对照组相比,STEMI患者编码精氨酸酶1的基因在入院时和STEMI后24-48小时的表达显著升高,但在三个月后则不再升高。编码精氨酸酶2和内皮NO合酶(NOS3)的基因的表达没有改变。精氨酸酶1蛋白水平在STEMI入院时、STEMI后24小时升高,并保持升高长达6个月。研究人员未观察到血浆精氨酸酶1蛋白水平与梗塞面积之间存在显著的相关性。
由此可见,入院时精氨酸酶1的基因和蛋白表达显著增加表明精氨酸酶1在STEMI发生发展中发挥着重要作用。
原始出处:
John Tengbom.et al.Arginase 1 is upregulated at admission in patients with ST-elevation myocardial infarction.J INTERN MED.2021.https://doi.org/10.1111/joim.13358
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#精氨酸#
68
#ST段抬高#
76
#Med#
62
#ST段#
77
棒棒棒,嗯嗯谢谢分享
91