Brit J Heamatol:同型半胱氨酸与镰状细胞病患者微血管病变的严重程度有关
2020-04-28 MedSci原创 MedSci原创
年龄和同型半胱氨酸浓度是SCD患者微血管病变的独立预测因子。
镰状细胞病(SCD)的病理生理学机制中包括血管病变和贫血。血浆同型半胱氨酸升高是血管疾病的危险因素,可能与SCD患者血管并发症的风险增加有关。
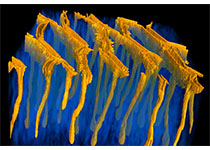
近日,血液系统疾病权威杂志British Journal of Haematology上发表了一篇研究文章,在该研究中,研究人员使用计算机辅助活体显微镜的无创性技术评估了18例小儿和18例成年SCD患者球结膜的微血管特征。研究人员计算了血管病变严重程度指数(SI)以量化每位患者的微血管病变程度,并测量了血浆同型半胱氨酸及其几个决定因素[血清叶酸和维生素B12、血浆磷酸吡哆醛(维生素B6的状态)和肌酐(肾功能)]。
年龄与SCD患者的微血管病变密切相关,年龄每增加1岁,SI升高约0.1个单位(P<0.001)。在调整了年龄、性别、维生素B状态和肌酐后,高半胱氨酸浓度与严重程度指数直接相关(P<0.05)。年龄和同型半胱氨酸浓度是SCD患者微血管病变的独立预测因子。
然而,使用适当的维生素B补充剂(叶酸和维生素B12和B6)降低同型半胱氨酸的浓度是否可以改善SCD患者的微血管病变及其相关并发症,仍有待进一步明确。
原始出处:
Sandra L. Samarron.et al.Homocysteine is associated with severity of microvasculopathy in sickle cell disease patients.british journal of haematology.2020.https://doi.org/10.1111/bjh.16618
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










系统性学习了
89
#血管病#
78
#微血管#
73
#血管病变#
65
#微血管病变#
71
#镰状细胞#
70