新冠肺炎致死真相:肾衰、心衰发生率远高于SARS,或与ACE2受体分布有关?
2020-02-15 Walter 转化医学网
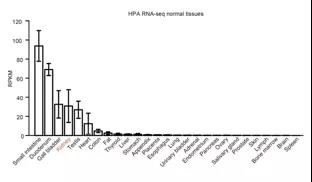
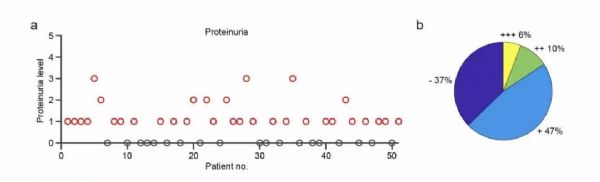
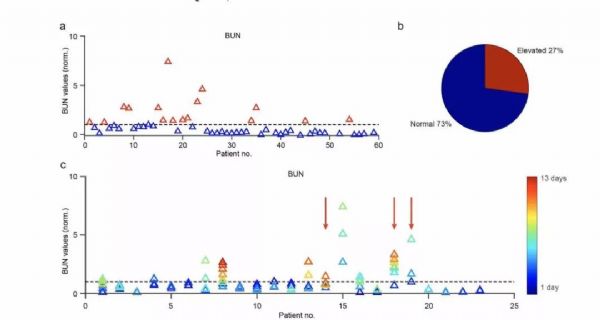
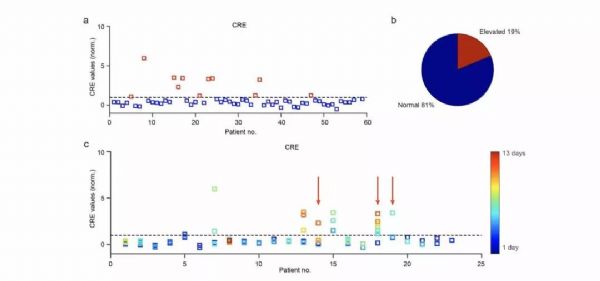
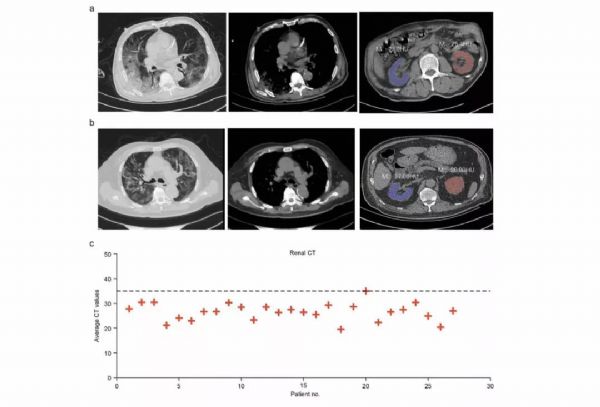
第三军医大学谌小维、周艺、鄢俊安及中国科学院苏州生物医学工程技术研究所贾宏博团队在医学预印本网站Medrxiv上发表结果,发现新冠肺炎的新临床特征:病例中肾功能衰竭的发生率远高于SARS,并强烈建议及时检测重症患者的肾功能,可能是大大降低死亡比例的关键。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ACE#
89
#发生率#
99
学习了
125
#SARS#
83
#ACE2#
94
我想知道某个脏器功能障碍时炎性因子水平。同时是否是动态观察水平?
115
新冠肺炎,疫情何时才能消失
90
希望早日攻克新冠肺炎
147
那后期的并发症是不是更多?
132