Spine J:新型混合融合手术可治疗成人腰椎侧弯
2014-04-16 佚名 丁香园
成人脊柱畸形的矫正常需行长节段脊柱融合至骶椎,手术并发症发生率高,多种原因可引起术后腰骶关节固定失败。目前常用的融合技术为第三代前后联合融合术,即前路松解加后路长节段固定至骨盆。但至今对于此挑战性手术,仍无理想的解决方案。研究表明,前路融合具有诸多优点,但由于大血管分叉而无法固定至骨盆。 美国纽约特殊手术医院脊柱与侧弯中心的学者进行了一项回顾性研究,提示新型混合融合手术可成功治疗成人腰椎侧弯
成人脊柱畸形的矫正常需行长节段脊柱融合至骶椎,手术并发症发生率高,多种原因可引起术后腰骶关节固定失败。目前常用的融合技术为第三代前后联合融合术,即前路松解加后路长节段固定至骨盆。但至今对于此挑战性手术,仍无理想的解决方案。研究表明,前路融合具有诸多优点,但由于大血管分叉而无法固定至骨盆。
美国纽约特殊手术医院脊柱与侧弯中心的学者进行了一项回顾性研究,提示新型混合融合手术可成功治疗成人腰椎侧弯,文章于2014年4月发表在Spine J上。
该病例-对照研究共纳入33对成人腰椎侧弯的连续病例,其中33例行新型混合融合手术,33例行传统前后联合融合术。新型混合融合技术为胸腹联合入路,间盘切除,融合器植入并以钉棒系统侧方固定至L3或L4;后方椎弓根钉棒系统固定融合L3/L4至S1。手术相光指标包括手术时间,失血量和融合节段。影像评估包括手术前后及随访的侧凸角度。临床疗效为SRS-22r和ODI指数。术后随访时间两组分别为5.3和4.6年。
研究结果显示,新型融合技术组在手术时间、失血量和融合节段上均低于传统前后联合融合组。两组病例术后胸弯角度无差异,但新型融合组对腰弯和腰骶弯(L4-S1)的矫形效果明显优于传统组。主要并发症(包括交界部位后凸、肺栓塞、内置物失败、深部感染和假关节)发生率,新型技术组明显低于传统组(18%对33)。
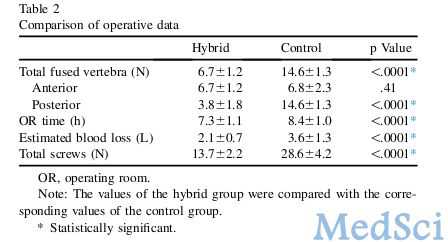
上述结果显示,新型融合技术长期疗效优良,其手术相关指标,包括手术时间、失血量和融合节段,及手术并发症,均低于传统的前路松解、后路融合至骶椎的手术技术。该技术既可节省融合节段,又能达到很好的矫形效果。
本研究为66例成人侧弯的回顾性分析,新型融合技术虽取得了良好的矫形效果,但其前路和后路固定融合有重叠,有带来并发症的可能。这些问题有待将来大样本、长期和多中心的研究加以证实。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
50
#腰椎#
47
#融合#
44