Science:牙周炎的原因终于搞明白了!迄今全面的牙周炎机制研究表明,口腔黏膜中促炎因子沉积是罪魁祸首!
2021-12-30 奇点网 奇点网
在某些情况下,纤维蛋白导致中性粒细胞免疫从保护性变为破坏性,这种纤维蛋白-中性粒细胞的相互作是牙周炎的驱动因素之一,因此有望成为严重牙周炎的防治靶点。
俗话说,“牙疼不是病,疼起来真要命”,引起广义上的牙疼的原因有很多种,其中之一就是牙周病,牙龈红肿或许好解决,但是严重的牙周炎会导致牙齿松动和脱落,这对生活的质量的影响可大了去了。
虽然科学家们已经知道了严重牙周炎是由过度的免疫反应引起的,但这种过度的免疫反应是如何发生的?它又是如何导致牙龈组织和牙槽骨受损的?这些问题都还没有答案。
在最近的《科学》杂志上,美国国立牙科和颅面研究所(NIDCR)的研究人员发表了一项新研究[1],他们发现,严重牙周炎中过度的免疫反应是由于纤维蛋白沉积在口腔粘膜中,招募并激活中性粒细胞,诱导活性氧(ROS)产生和中性粒细胞外陷阱的形成(NETosis)导致的。抑制纤维蛋白沉积或NETosis可能是治疗严重牙周炎的关键靶点。
纤维蛋白是一种促炎因子,与血栓形成和炎症有关。过去的研究发现,纤维蛋白在口腔黏膜中的病理性沉积会导致严重的牙龈组织和牙槽骨的受损,导致青少年整个齿列的缺失[2,3],而齿列周围的粘膜炎症和牙槽骨损伤正是牙周炎的标志。
纤维蛋白沉积由纤溶酶负责消除,因此在出现病理性沉积的患者中通常存在纤溶酶的缺失。因此,研究人员做出了假设,即,纤溶酶介导的纤维蛋白溶解的缺失可能是牙周炎患者口腔黏膜过度免疫反应的原因。
为了验证这个假设,他们开始一系列实验。
首先,研究人员构建了蛋白纤溶酶原(PLG,纤溶酶的前体)和纤维蛋白原(纤维蛋白的前体)双缺失的小鼠,和同窝的PLG缺失/纤维蛋白原部分缺失的小鼠相比,前者完全没有纤维蛋白的沉积,而且,纤维蛋白原缺失也完全避免了PLG缺失会导致的牙槽骨的损伤。这就表明,PLG缺失引起的口腔黏膜过度免疫反应是由纤维蛋白沉积驱动的。

PLG和纤维蛋白原双缺失小鼠(右下)和同窝PLG缺失/纤维蛋白原部分缺失小纤维蛋白的沉积情况
在PLG缺失,纤维蛋白沉积的小鼠的口腔黏膜(牙龈)组织中,研究人员发现了大量的中性粒细胞,相应的,负责中性粒细胞招募和粒细胞生成的基因、参与中性粒细胞和单核细胞活化的基因表达都大大增加。中性粒细胞的数量不仅在整个病理周期中的每一个时间点都显著增加,还是唯一一种在病理阶段早期(12周)也增加的细胞亚群。
整合素αMβ2是介导中性粒细胞招募的重要分子,整合素家族的成员也在介导细胞间和细胞与细胞外基质间的黏附方面发挥重要作用。实验显示,αMβ2介导了中性粒细胞和纤维蛋白的黏附,诱导活性氧(ROS)产生和中性粒细胞外陷阱的形成(NETosis)。
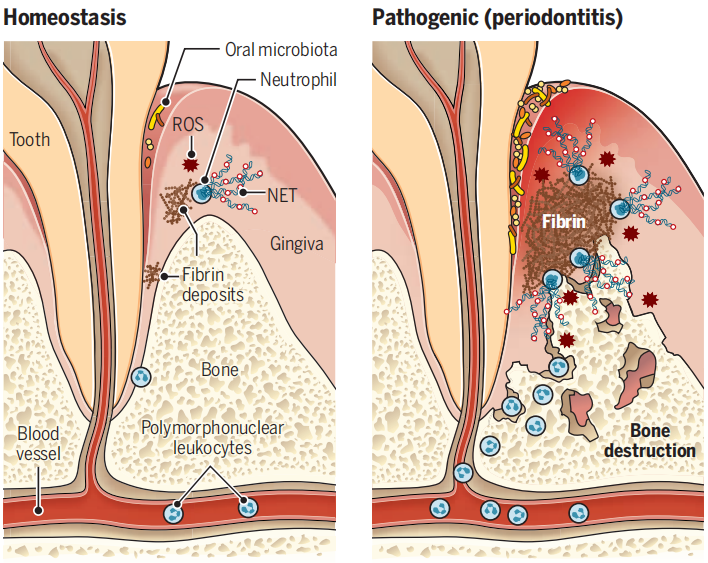
当研究人员通过药理学或者遗传学手段抑制了PLG缺失小鼠细胞外DNA和NETosis的积累时,小鼠牙槽骨的损伤显著减轻。同样,利用小干扰RNA(siRNA)靶向消除纤维蛋白原后,也显著减轻了牙槽骨的损伤。
不仅仅是PLG缺失的特殊小鼠,在自然衰老的野生型小鼠中,纤维蛋白无法沉积的小鼠随年龄增长而自发出现的牙槽骨损伤也明显比同窝的对照组小鼠要轻。
因此,纤维蛋白沉积和NETosis都是阻止严重牙周炎导致的牙槽骨损伤的重要靶点。
研究人员在牙周炎患者的牙龈组织中也发现了同样高水平的纤维蛋白沉积和中性粒细胞浸润,而健康人中则几乎没有。
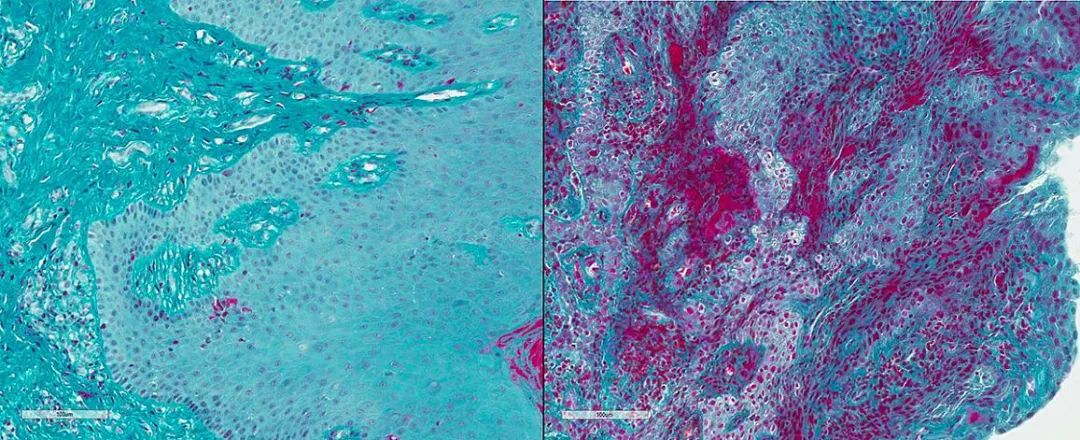
健康人(左)和牙周炎患者(右)牙龈组织中纤维蛋白(红色)的沉积对比
此前在欧洲进行的全基因组关联研究曾提出过,PLG(rs1247559)下游多态性与侵袭性牙周炎相关[4,5],研究人员也在他们的牙周炎患者队列中验证了这一发现,他们发现,PLG(rs2465836)与严重牙周炎和一种牙周炎相关病原体,伴放线菌团聚杆菌的高度定植有关。
也就是说,即使不会导致严重的PLG缺失,PLG基因的单核苷酸变异也与严重的牙周炎风险增加有关。这也意味着在小鼠中发现的免疫机制可能在人类患者中也同样适用。
研究的通讯作者之一,Niki Moutsopoulos博士表示,这项研究表明,在某些情况下,纤维蛋白导致中性粒细胞免疫从保护性变为破坏性,这种纤维蛋白-中性粒细胞的相互作是牙周炎的驱动因素之一,因此有望成为严重牙周炎的防治靶点,也可能为其他以纤维蛋白沉积为特征的炎症性疾病,例如部分关节炎和多发性硬化症提供新的治疗思路。
参考文献:
[1]https://www.science.org/doi/10.1126/science.abl5450
[2] Waschulewski I K, Gökbuget A Y, Christiansen N M, et al. Immunohistochemical analysis of the gingiva with periodontitis of type I plasminogen deficiency compared to gingiva with gingivitis and periodontitis and healthy gingiva[J]. Archives of oral biology, 2016, 72: 75-86.
[3] El‐Darouti M, Zayed A A, El‐Kamah G Y, et al. Ligneous conjunctivitis with oral mucous membrane involvement and decreased plasminogen level[J]. Pediatric dermatology, 2009, 26(4): 448-451.
[4] Munz M, Richter G M, Loos B G, et al. Meta-analysis of genome-wide association studies of aggressive and chronic periodontitis identifies two novel risk loci[J]. European Journal of Human Genetics, 2019, 27(1): 102-113.
[5] Schaefer A S, Bochenek G, Jochens A, et al. Genetic evidence for PLASMINOGEN as a shared genetic risk factor of coronary artery disease and periodontitis[J]. Circulation: Cardiovascular Genetics, 2015, 8(1): 159-167.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#机制研究#
160
#促炎#
98
#促炎因子#
103
学习学习
90
学习
91
涨知识了
86
学习
104
学习新知识了
138
#SCIE#
70
#牙周#
99