欧盟授予CM-101治疗原发性硬化性胆管炎的孤儿药资格
2020-08-31 Allan MedSci原创
原发性硬化性胆管炎(primary sclerosing cholangitis, PSC)是一种不明病因的慢性进展性疾病,其特征是肝内和/或肝外胆道系统内中型和大型胆管发生炎症、纤维化及狭窄。英国一
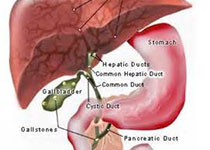
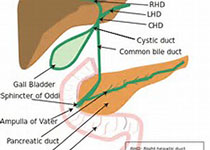
原发性硬化性胆管炎(primary sclerosing cholangitis, PSC)是一种不明病因的慢性进展性疾病,其特征是肝内和/或肝外胆道系统内中型和大型胆管发生炎症、纤维化及狭窄。英国一项研究显示,1998-2014年,PSC发病率为0.68/100,000人年,年龄标准化患病率为5.58/100,000人年。

生物技术公司Chemomab今日宣布,欧洲委员会(EC)根据欧洲药品管理局(EMA)孤儿药物产品委员会(COMP)的积极意见,已授予其主要候选药物CM-101治疗原发性硬化性胆管炎(PSC)的孤儿药资格(ODD)。先前,CM-101已获得美国食品和药品监督管理局(FDA)的ODD。CM-101是一种CCL24封闭性单克隆抗体,具有减轻纤维化和炎症的作用。CM-101干扰了促进纤维化和炎症的主要病理过程。如多项体内、体外和离体研究所示,CM-101在改善纤维化方面非常有效。
Chemomab首席执行官Adi Mor博士说:“ODD是CM-101的全球发展计划的重要里程碑。来自CM-101的I期临床试验的数据令人鼓舞,并表明CM-101是安全的,具有抗纤维化的临床功效。我们期待在2020年第三季度开始IIa期临床试验。目前尚无经过批准的PSC治疗方法,因此迫切需要开发新的治疗方法以改善患者的生活质量”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#原发性#
85
#CM-101#
58
#原发性硬化性胆管炎#
105
#硬化性#
52
#胆管#
52
学习
112