J Crohns Colitis:克罗恩病肛周瘘相关癌患者的特征及临床预后
2021-04-03 Nebula MedSci原创
克罗恩病肛周瘘相关癌患者的特征及临床预后
肛周瘘是克罗恩病(CD)患者的特征性并发症。CD患者发生任何类型瘘的10年和50年累积风险分别是33%和50%,其中发生肛周瘘的风险分别是21%和26%。
肛周瘘相关癌是CD患者面临的一个未被充分研究的风险。本研究旨在提高临床对CD患者肛周瘘相关癌的认识,促进诊断和治疗策略的发展。
这是在德国四家医院进行的回顾性病例对照研究,纳入了40名确诊为与肛周克罗恩氏瘘相关的恶性肿瘤患者和40名随机选择的发生了肛周瘘的CD对照患者。分析了各组之间的差异,并进行多变量评估,以描述肿瘤预后相关的危险因素。
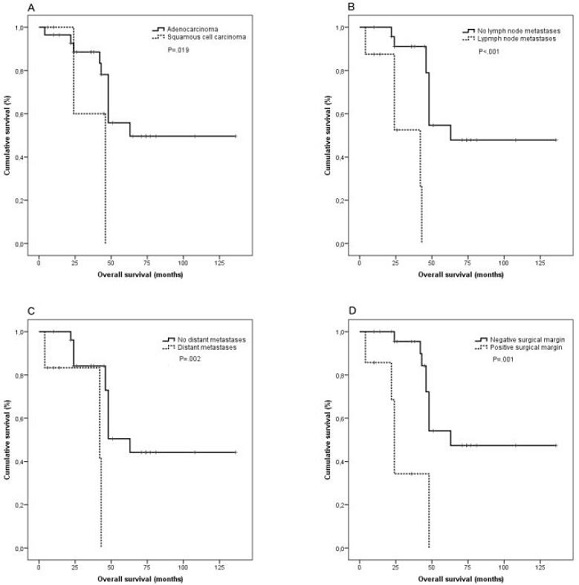
根据组织学类型、淋巴结转移、远处转移和手术边缘分层的患者的总生存率
40位恶性肿瘤患者中有33例为腺癌,7例为鳞癌。与无癌的肛周瘘CD患者相比,与瘘管相关的恶性肿瘤患者确诊为克罗恩病时的年龄更小。恶性肿瘤患者克罗恩病持续时间较长(25.8±9.0 vs 19.6±10.4年;p=0.006)。
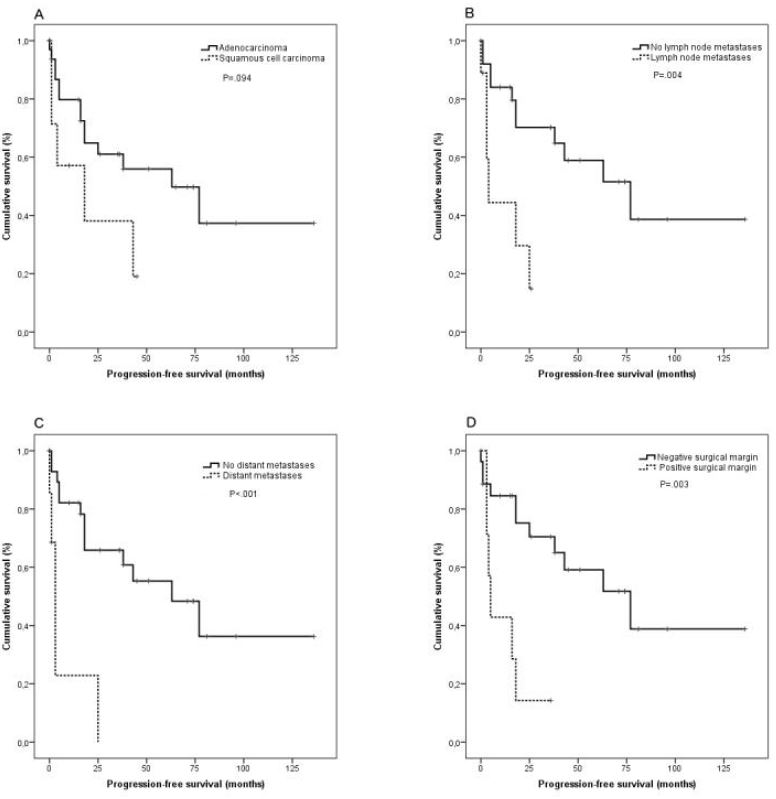
根据组织学类型、淋巴结转移、远处转移和手术边缘分层的患者的无进展存活期
两组与瘘管相关的发现有显著差异。复杂和严重的瘘管征象,包括复杂的解剖结构和慢性活动性,在与瘘管相关恶性肿瘤患者中明显更常见。显著影响瘘管相关恶性肿瘤患者总体死亡率和无进展生存率的风险因素有肿瘤的组织类型、有无转移和R1期切除。在本试验中,瘘管相关恶性肿瘤患者的总生存期(OS)为45.1±28.6个月,5年生存率为65%。
总之,在克罗恩病合并肛周瘘的腺癌或鳞癌患者中,瘘管特征决定了恶性肿瘤的风险。早期诊断影响预后,而慢性瘘管活动的治疗可能是预防恶性肿瘤的关键。此外,专家多模式治疗是成功治疗肛周瘘管相关恶性肿瘤的关键。
原始出处:
Palmieri Chiara,Müller Gerhard,Kroesen Anton J et al. Perianal fistula-associated carcinoma in Crohn′s disease: a multicenter retrospective case control study. J Crohns Colitis, 2021, https://doi.org/10.1093/ecco-jcc/jjab057
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肛周瘘#
66
#Crohn#
62
#CRO#
43
#colitis#
64
#临床预后#
49