Sci Rep:系统性硬化症胃黏膜凋亡和增殖因子的表达与疾病类型有关
2019-12-10 xiangting MedSci原创
这项研究数据表明sys1是SSc最“活跃”的增殖形式。Sys2特征是胶原蛋白沉积、表面上皮缺陷、广泛的凋亡和低增殖、GM萎缩和功能丧失。
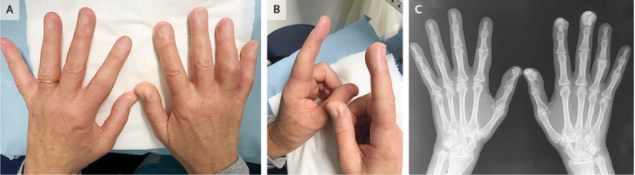
尽管系统性硬化症患者(SSc)中胃病的患病率很高,但人们对其发病机理仍知之甚少。
研究人员通过免疫组化分析了5名对照和15名不同形式SSc患者的胃黏膜活检(GM):局灶性皮肤病(lc)、中度弥漫性皮肤病(sys1)和重度弥漫性皮肤病(sys2)。通过Kruskall-Wallis检验分析阳性细胞数,P<0.05被认为具有统计学意义。
sys1患者的增殖细胞(Ki-67阳性)百分比最高(表层的3%,GM较深部分的4.6%),sys2患者降至1%。对照组α-平滑肌肌动蛋白(α-SMA)阳性细胞的百分比为5%,占表层GM的9%,而sys1和sys2患者较深GM的阳性细胞从7%升至19%,从而表明成肌纤维细胞数量增加。在sys1患者中,Caspase-3阳性凋亡细胞占对照组的1.5–2%,浅表的8%和深层GM的6%。在sys2中,凋亡影响了50%的表面上皮细胞和腺细胞以及30%的较深腺体,并与纤维化增加和多配体蛋白聚糖-1表达降低相关。
这项研究数据表明sys1是SSc最“活跃”的增殖形式。Sys2特征是胶原蛋白沉积、表面上皮缺陷、广泛的凋亡和低增殖、GM萎缩和功能丧失。
原始出处:
Katarina
Boric. Expression of apoptotic and proliferation factors in gastric mucosa of
patients with systemic sclerosis correlates with form of the disease. Sci Rep.
05 December 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
39
#胃黏膜#
51
#硬化症#
43
学习了谢谢分享
93
#黏膜#
51
#系统性硬化#
41