一、病史简介
女性,28岁,浙江人,2018-02-08入中山医院感染病科
主诉:发现颈部肿块9月,伴反复咳玉米碎样物1月
现病史:
患者于2017-05初出现右侧颈部肿痛,自扪及右颈部中段卵圆形包块1枚,直径约3*2cm,质韧,移动度差,压痛明显,皮温不高,无咽痛、咳嗽、咳痰、发热、盗汗等不适。2017-05-11于我院就诊,查WBC 6.36*10^9/L,N% 59.7%,hs-CRP 4.0mg/dl,ESR 24mm/h,T-Spot A/B 89/116;颈部超声示:右侧颈部淋巴结肿大(最大37×11mm);左侧颈部见淋巴结(最大16×6mm);胸部CT示:左肺下叶病变,慢性及陈旧炎性病变可能;行超声引导下右颈部淋巴结穿刺,吸出少量黄色粘稠液体,涂片见大量凝固性坏死,部分炎症细胞,结核性坏死不能除外。
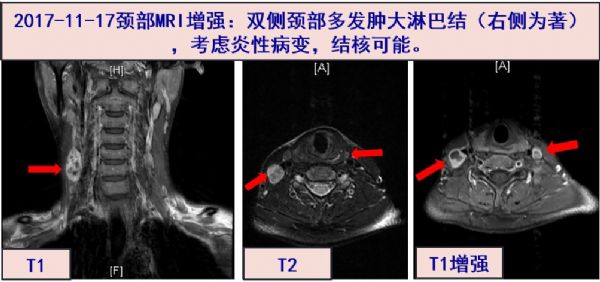
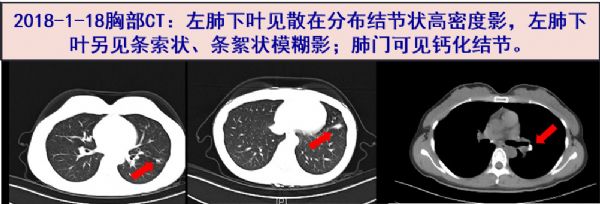
2017-05-17起予以异烟肼0.3g qd+利福平0.45g qd+吡嗪酰胺0.5g tid+乙胺丁醇0.75g qd抗结核治疗,自觉颈部肿物渐缩小,疼痛缓解,随访炎症指标正常范围。08-22停用吡嗪酰胺。09-22复查T-Spot A/B 39/107,超声示颈淋巴结肿大较前缩小。 2017-11-17颈部MRI增强:双侧颈部多发肿大淋巴结(右侧为着)。2018-1-18胸部CT:左肺下叶见散在分布结节状高密度影,左肺下叶另见条索状、条絮状模糊影;肺门可见钙化结节。
2018-01开始出现有咽部异物感,并咳出“玉米碎样物”至少4次,色黄,质地偏软,未予重视和检查;
2018-02-07复查超声,仍示右侧颈部淋巴结肿大(部分融合成团,最大28×13mm),左侧颈部见淋巴结(最大12×4mm),考虑抗结核效果不佳,次日收入我科进一步检查。
既往史及个人史:2016-11 行拔牙术。
二、入院检查(2018-2-8)
体格检查:
T 36.5℃,P 90bpm,R 18次/分,BP 122/84mmHg
右侧颈部触及数枚肿大淋巴结,大者长径2cm左右,质韧,移动度差,有压痛,余浅表淋巴结未及肿大。全身皮肤无皮疹,无瘀点瘀斑。双侧扁桃体未见明显肿大。两肺呼吸音请,未闻及明显啰音。腹部平软,无压痛,肝脾肋下未及。
实验室检查:
血常规:WBC 5.41X10^9/L,N 60.4%,L 29%;
炎症标志物:CRP 1.9mg/L;ESR 16mm/H;PCT 0.07ng/mL;
肝肾功能电解质:均正常;
出凝血功能:均正常;
三、临床分析
病史特点:青年女性,颈部肿痛起病,病程长达9个月。近一个月出现咽部异物感,并多次咳出“玉米碎样物”。无发热、咳嗽等症状。血炎症指标水平正常,T-SPOT明显升高,淋巴结细针穿刺涂片见大量凝固性坏死,抗结核治疗8月余,但淋巴结缩小不明显。诊断和鉴别诊断考虑如下:
颈淋巴结肿大 慢性病程,病理见肉芽肿伴坏死,T-SPOT显着升高,首先考虑结核感染。标准抗结核治疗后淋巴结肿大改善不明显,要考虑淋巴结中抗结核药物浓度低,或耐药结核菌感染导致临床效果不佳之可能,也有可能其他病原体如非结核分枝杆菌(NTM)引起的可能。可再次行淋巴结活检和微生物检查,必要时调整抗感染治疗方案。淋巴瘤或肿瘤转移引起颈淋巴结肿大,依据不足。
气道或肺部病变 患者自诉多次咳出“玉米碎样物”,是否为肺或气道内组织感染(如曲霉菌)或肿瘤坏死脱落?或是“硫磺样”颗粒?需要仔细询问病史,以及留取“玉米碎样物”进行肉眼观察、显微镜检查(病理学和微生物形态学)和基因检测(mNGS)。“硫磺样”颗粒被认为是放线菌感染具有一定特征性表现。但仔细阅读1月18日胸部CT,两肺未见明显活动性病灶。当然可以做内镜检查如支气管镜和喉镜检查,以防止腔道内病灶不容易被CT识别而导致疾病诊断遗漏。此外,颈淋巴结肿大和咳出“玉米碎样物”,是同一种疾病还是各不相关的两种疾病,目前资料尚不能明确鉴别。
四、进一步检查、诊治过程和治疗反应
2018-02-09 超声引导下颈部淋巴结穿刺活检及微生物培养。
2018-02-09 嘱出院,继续予以异烟肼、利福平和乙胺丁醇三联抗结核治疗。待病理和微生物报告。
出院后随访

出院后3天再次咳出玉米碎样物,呈黄白色(如图)。留标本送二代测序(mNGS)检查。
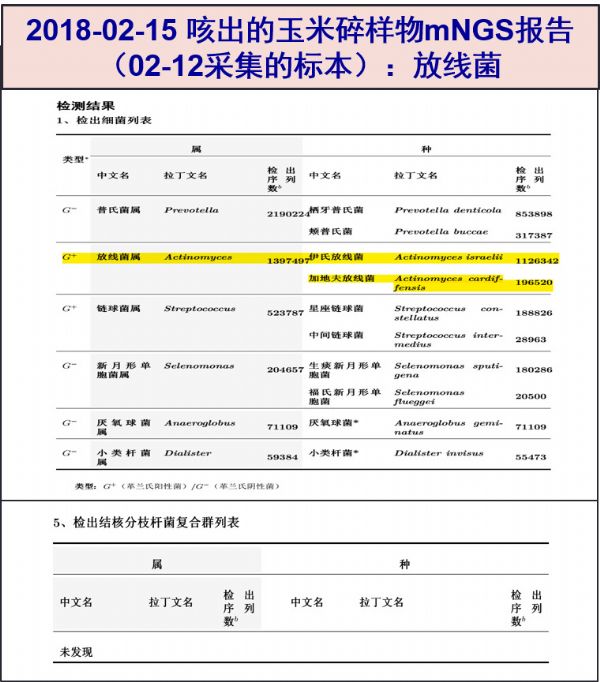
02-15 mNGS报告,检测到大量“伊氏放线菌”核酸序列,未发现结核分枝杆菌核酸序列。
出院后随访(再次入院)
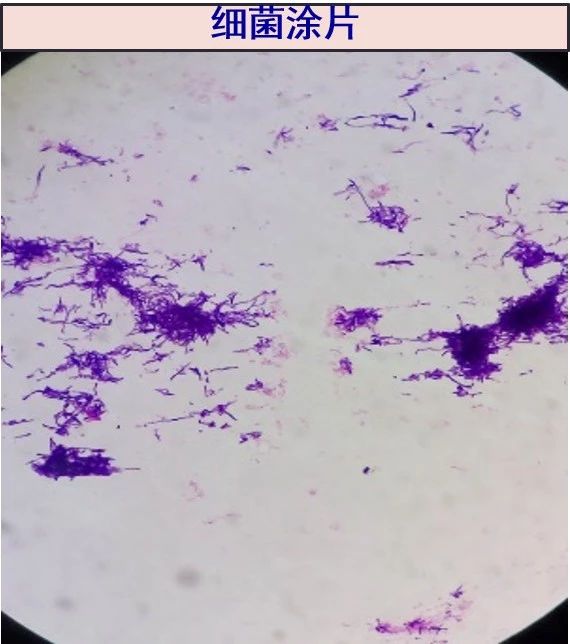
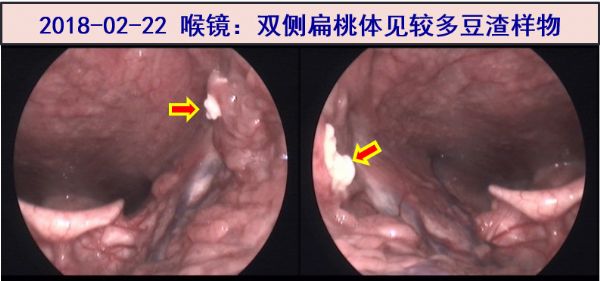
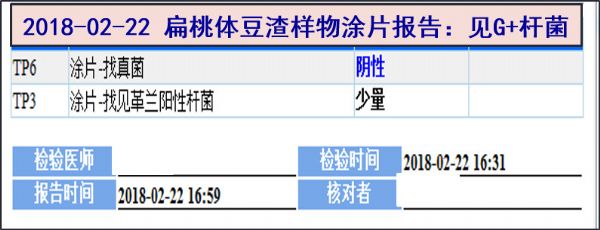
2018-02-22 春节长假(02-15至02-21)过后再次收住入院。当天喉镜检查:双侧扁桃体见较多豆渣样物,部分深入粘膜下,送常规微生物检查、二代测序(mNGS)及组织病理检查。当天微生物实验室涂片报告:见革兰阳性杆菌,抗酸杆菌阴性;
02-22 颈部淋巴结病变仍考虑为结核,故继续予以异烟肼、利福平、乙胺丁醇治疗;
02-23 复查颈部淋巴结超声:右侧颈部见多个低回声团块,部分融合成团,最大22×12mm,左侧颈部未见明显肿块回声,淋巴结肿大较02-07好转;
02-23 第一次咳出物二代测序结果检出大量放线菌核酸序列、本次细菌涂片为革兰阳性杆菌,考虑放线菌可能大,开始予以青霉素480万U q8h 静脉治疗。
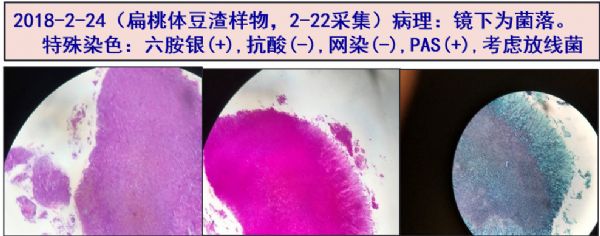
02-24 扁桃体豆渣样物病理报告:镜下为菌落。特殊染色:六胺银(+),抗酸(-),网染(-),PAS(+),考虑放线菌。
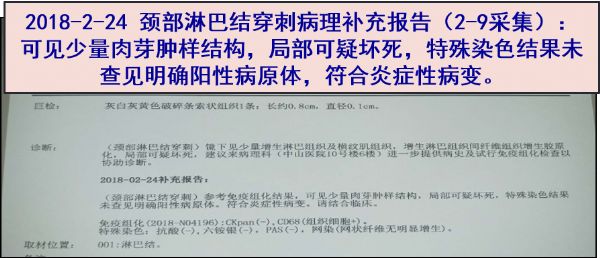
02-24 (02-09送检)颈部淋巴结穿刺病理补充:可见少量肉芽肿样结构,局部可疑坏死。
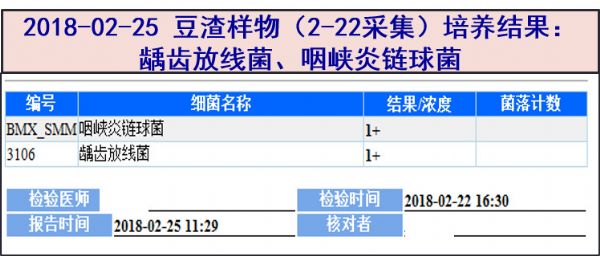
02-25 (扁桃体豆渣样物,2-22采集)细菌培养: 龋齿放线菌、咽峡炎链球菌。
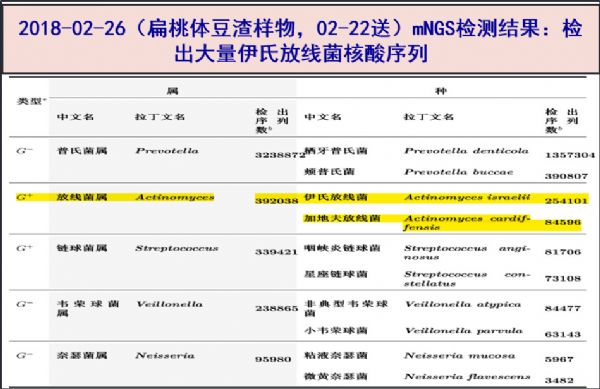
02-26 (豆渣样物,2-22采集)mNGS检测报告:伊氏放线菌大量核酸序列。
03-02 喉镜提示扁桃体豆渣样物较前减少。予出院治疗,调整抗感染方案为:口服异烟肼+利福平+乙胺丁醇+莫西沙星抗结核、阿莫西林抗放线菌治疗。
03-22 咽部异物感消失,也未再有玉米碎样物咳出。门诊复查喉镜:扁桃体未见豆渣样物质。但仍有颈部淋巴结肿大伴疼痛,建议继续抗结核治疗,必要时可考虑外科淋巴结切除。随访中......
五、最后诊断与诊断依据
最后诊断:
扁桃体放线菌感染
颈淋巴结结核
诊断依据:
青年女性,有咽部异物感,多次咳出玉米碎样物。喉镜检查双侧扁桃体见“豆渣样物”,部分深入粘膜下。摘除后病理检查,镜下考虑放线菌,特染六胺银(+),PAS(+),抗酸(-) 。2次mNGS检测均检出大量“伊氏放线菌”核酸序列。微生物检查,涂片见革兰阳性杆菌,细菌培养为“龋齿放线菌”。予大剂量青霉素静滴、后续阿莫西林口服治疗,4周后复查喉镜扁桃体豆渣样物消失,故诊断扁桃体放线菌感染可以成立,综合临床过程,感染程度较轻。至于感染病原体菌种,究竟是伊氏放线菌还是龋齿放线菌,从目前资料不能完全区分。一般认为伊氏放线菌致病力相对较高,而且核酸检测的准确性也较好。
同时,患者颈部淋巴结肿大10月余,T-SPOT强阳性,曾淋巴结细针穿刺涂片见大量凝固性坏死,虽然标准抗结核治疗后淋巴结缩小不够明显,但再次穿刺活检病理仍提示见肉芽肿样结构,局部可疑坏死,淋巴结组织二代测序也无放线菌证据,且大剂量静滴青霉素G和后续口服阿莫西林治疗,扁桃体病变消失但颈部淋巴结仍无明显缩小,疼痛感依存,故仍考虑同时合并颈部淋巴结结核可能大。
六、经验与体会
放线菌病是一种少见的感染性疾病。常见病原菌包括有伊氏放线菌(A. israelii)、牛放线菌、内氏放线菌、黏液放线菌和龋齿放线菌(A. odontolyticus)等。一般定植于人和动物的口腔、上呼吸道、胃肠道和泌尿生殖道。放线菌感染需要链球菌等伴生菌的协助,如消耗氧气、破坏粘膜屏障而促进放线菌侵入。该菌感染引起的病理改变为化脓性、肉芽肿性病变,六胺银染色及PAS均阳性。临床工作中放线菌的培养阳性率低,主要与抗生素广泛应用、培养条件不够(接种时无法维持厌氧环境、培养时间短)有关。放线菌致病力弱,不具有传染性,在口腔卫生差、免疫力低下等情况下,粘膜或上皮屏障功能破坏时可侵入受损组织致病,且易侵袭周围组织。
目前根据感染部位将放线菌感染分为头颈型(60%)、胸型和腹盆型。其中头颈型感染常见的危险因素包括拔牙、龋齿、酗酒、营养不良等,约50%的病例为上颌骨和下颌骨周围软组织感染。放线菌感染的确诊主要靠组织培养或组织病理切片找到放线菌。
本例患者最初是咳出物(玉米碎样物)送二代基因测序(mNGS),发现大量放线菌核酸序列才获得重要线索。之后进一步检查发现扁桃体病变,采集标本做涂片、培养、病理检查、复查mNGS,才明确放线菌感染诊断。
放线菌感染累及扁桃体见于5岁以上儿童和成年人,多表现为反复的扁桃体炎、扁桃体肿大等,有个案报道扁桃体放线菌感染见类似结石样物质。本例喉镜检查时,ENT医生最先描述为“扁桃体结石”,活检发现病变组织质地软,改称为“豆渣样物”,后续检查提示放线菌感染,属罕见病例。本例患者描述咳出的“玉米碎样物”,实验室检查为“放线菌菌团”,应视为文献介绍的“硫磺样颗粒”。硫磺样颗粒(Sulfur granule)是放线菌感染特征性表现,呈肉眼可见的黄色小颗粒状菌落,系菌丝与蛋白-多糖复合物,而无任何硫磺成分。将硫磺样颗粒制成压片或组织切片,在显微镜下可见颗粒呈菊花状,由棒状长丝呈放射状排列组成,本例病理切片(见附图)镜检也看到典型的放射状排列的长丝。
放线菌感染首选抗菌药物治疗,外科手术作为辅助。一般无需行药敏试验。首选青霉素类药物,无外科干预情况下抗感染疗程通常为6-12个月。仅短期抗菌治疗,扁桃体放线菌感染易反复,甚至需行扁桃体切除。本例患者在明确诊断后,立即应用大剂量青霉素治疗,短期内效果明显;患者初次发作,不考虑外科治疗。因为病情轻、病灶范围小,抗感染治疗1月病灶基本消失,我们认为治疗疗程应该可以短于文献报告的6-12月。
文献报告放线菌导致淋巴结感染的病例不多,主要通过淋巴结活检病理确诊。该例淋巴结肿大抗结核治疗效果不佳,但组织活检病理未提示放线菌感染证据,且青霉素治疗后扁桃体病变消失而颈部淋巴结肿大无明显缩小,故不考虑放线菌淋巴结累及。
原始出处
[1] Cohen PR, et al. Tonsillaractinomycosis mimicking a tonsillolith: colonization of the palantine tonsilpresenting as a foul-smelling, removable, unilateral, giant tonsillarconcretion. Int J Dermatol. 2010 Oct;49(10):1165-8.
[2] Arik D. Actinomyces lymphadenitis: casereport. Turk Patoloji Derg,2013;29(1):80-2.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#基因技术#
126
#肿块#
108
#颈部#
79
技术进步的又一个体现
174
谢谢了.学习
132
看看了解一下了
174
了解了解.学习学习
137
学了
120
学习了.谢谢分享
132
好好好好好好好好
118