心脏是一台泵血的“发动机”,它将血液输送到肺进行气体交换,然后再将充满氧气的血液“泵”向全身各器官以维持生命。它也是一台有节律的“精密的仪器”,由具有精确协调的“电路系统”来启动和维持心脏正常而有节律的跳动。
心脏分为左、右心房和左、右心室。位于右心房上部的窦房结规律地发放脉冲指令。窦房结每发生一次冲动,心脏就跳动一次,在医学上称为“窦性心律”。它是人体正常心律,频率在每分钟60-100次。
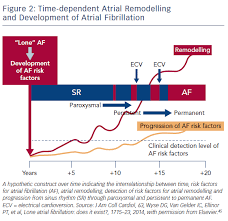
心房颤动简称房颤,是临床上最常见的一种持续性心律失常。房颤时,心房失去了正常有效的收缩功能,处于快速紊乱的颤动状态,频率可以快到300-600次/分钟,心室跳动快速而不规律,可达到100-200次/分钟。
房颤的发病率随着年龄增加而增高。大约1%的患者年龄<60岁,而75-84岁年龄组的发病率高达12%。同时,房颤还可以导致发生卒中的风险增加5倍,死亡率增高2倍;与房颤相关的卒中较非房颤相关的卒中更严重,房颤导致发生心衰的风险增高3倍,发生痴呆的风险增高2倍。
因此,筛查无症状的房颤患者并及时进行抗凝治疗对于预防卒中尤为重要。为此,来自加拿大和德国的心脏病学专家团队,联合开展了一项RCT,旨在评价2种基于家庭的房颤筛查干预措施效果。相关结果发表在最新的JAMA Cardiology杂志上。
这是一项多中心随机临床试验,招募了来自75岁以上高血压且无已知房颤的老年人。从2015.04.05-2019.03.26期间,共有来自48家诊所的856名参与者被纳入。对照组接受标准护理(常规临床随访加基线和6个月的脉搏检查和心脏听诊)。筛查组除接受标准护理外,还在基线和3个月时佩戴为期2周的连续心电图(cECG)贴片监测仪。筛查组还接受了具有振荡心房颤动筛查功能的自动家用血压(BP)机,在cECG监测期间每天使用两次。
研究的主要结局指标是通过意向性筛查分析,在6个月内由cECG监测或临床发现心房颤动。次要结果包括抗凝剂的使用、设备依从性和BP监测仪检测到的心房颤动。
结果显示,856名参与者中,487名为女性(56.9%);平均(SD)年龄为80.0(4.0)岁。cECG佩戴时间中位数为27.4天。在主要分析中,筛查组434名参与者中有23名(5.3%)检测到房颤,而对照组422名参与者中有2名(0.5%)检测到房颤(RR=11.2;绝对差异=4.8%;筛查所需数量=21)。
其中,在cECG检测到房颤的患者中,房颤的中位总时间为6.3h(IQR,4.2-14.0h),最长房颤发作的中位持续时间为5.7h(IQR,2.9-12.9h)。在20例cECG检测到房颤的患者中,有15例(75.0%)开始了抗凝治疗。到6个月时,筛查组434名参与者中的18名(4.1%)与对照组422名参与者中的4名(0.9%)已开出抗凝治疗处方(RR=4.4;绝对差异=3.2%)。
进一步分析显示,每天两次使用家庭血压监测仪进行房颤筛查的敏感性为35.0%,特异性为81.0%,阳性预测值为8.9%,阴性预测值为95.9%。在434名参与者中,有5人(1.2%)发生了需要过早停止cECG监测的不良皮肤反应。
综上,该研究显示,使用可穿戴式cECG监测仪进行房颤筛查的耐受性很好,可将房颤检出率提高10倍,并在大多数情况下促使患者尽早开始抗凝治疗。
参考文献:
Gladstone DJ, et al. Screening for Atrial Fibrillation in the Older Population: A Randomized Clinical Trial. JAMA Cardiol. Published online February 24, 2021. doi:10.1001/jamacardio.2021.0038
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cardiology#
73
#检出率#
99
#Cardiol#
81
#穿戴式#
68
#心衰风险#
75
#ECG#
79
#CEC#
74
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
76
房颤,临床上碰到很多哦
89
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
69